Introduction What We Can Offer? Why Choose Us? FAQs Featured Services Featured Products
Accelerate Your Research and Development!
Are you currently facing long drug development cycles, challenges in identifying effective targets for neuroprotection, or difficulty in developing highly specific therapeutics for complex neurological conditions? Creative Biolabs' comprehensive Complement System Therapeutic solutions help you accelerate drug discovery, obtain high-quality research tools, and develop highly specific antibodies through advanced recombinant protein technology, high-throughput screening platforms, and innovative antibody engineering techniques.
Contact our team to get an inquiry now!
Introduction
Acute ischemic stroke (AIS) constitutes a catastrophic neurological occurrence arising from abrupt cerebral blood flow cessation, inducing neuronal demise. Although reperfusion treatments are vital for reestablishing circulation, consequent ischemia-reperfusion (I/R) damage frequently intensifies cerebral injury. A pivotal mediator of this secondary pathology is complement cascade activation, a fundamental constituent of innate immunity.
Complement System in Acute Ischemic Stroke
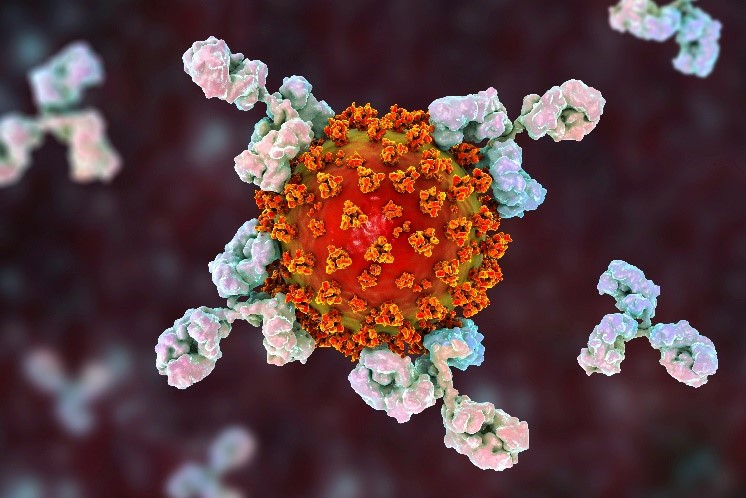
The complement system is a cascade of plasma proteins that, upon activation, plays a vital role in host defense by eliminating pathogens and clearing cellular debris. It consists of three main activation pathways: the classical, alternative, and lectin pathways, all converging at the activation of C3 and C5, leading to the formation of the Membrane Attack Complex (C5b−9) and the release of potent anaphylatoxins like C3a and C5a. While essential for immunity, uncontrolled or inappropriate complement activation can lead to tissue damage.
In the context of AIS, complement activation is rapidly initiated post-ischemia, particularly during reperfusion. Studies have shown that complement components, including C1q, C3, and C5, are deposited in ischemic brain tissue. The activation of these pathways contributes significantly to the inflammatory cascade, leading to:
-
Blood-Brain Barrier (BBB) Disruption: Anaphylatoxins C3a and C5a increase vascular permeability, contributing to brain edema and leukocyte infiltration.
-
Inflammation and Leukocyte Recruitment: C3a and C5a act as potent chemoattractants, recruiting neutrophils and macrophages to the ischemic site, further exacerbating inflammation and oxidative stress.
-
Direct Neuronal Damage: The formation of the MAC (C5b−9) on neuronal and glial cell membranes can lead to direct cell lysis. Furthermore, sublytic MAC can induce intracellular signaling pathways that contribute to apoptosis and necrosis.
-
Microglial Activation: Complement components, particularly C1q and C3b, can opsonize damaged neurons and synapses, leading to their phagocytosis by activated microglia, potentially contributing to neuronal loss in the penumbra.
The dual nature of the complement system – protective in host defense but detrimental in pathological conditions like AIS – highlights its potential as a therapeutic target. Modulating specific complement pathways or components offers a promising strategy to mitigate secondary brain injury and improve neurological outcomes after ischemic stroke. Research indicates that inhibiting complement activation, particularly at the C3 or C5 level, can reduce infarct volume and improve functional recovery in preclinical models of stroke.
 Fig.1 Schematic diagram of the triggers of complement activation after cerebral ischemia-reperfusion injury.1
Fig.1 Schematic diagram of the triggers of complement activation after cerebral ischemia-reperfusion injury.1
What We Can Offer?
Creative Biolabs is your comprehensive partner for advancing research and therapeutic development in complement system modulation for acute ischemic stroke, offering high-quality products and specialized services to support every project stage:
Products
|
Complement Proteins
|
High-purity, functionally active proteins (e.g., C1q, C5B-9, C3, C5, Factor B, Factor D, Properdin) for pathway reconstruction and functional assays.
|
|
Complement Component Antibodies
|
High-specificity monoclonal and polyclonal antibodies for detection, quantification, and functional studies (inhibition/activation).
|
|
Complement Inhibitors
|
Curated small molecules and biologics to modulate complement pathway activity, useful for mechanistic studies and drug screening.
|
|
Complement-Related ELISA Kits
|
Ready-to-use kits for quantitative detection of complement components, activation products, and regulators in various samples.
|
|
Complement Sera and Plasmas
|
Featured complement activity-preserved products are available for biocompatibility experiments, including drug development, biomaterials testing, lymphocytotoxicity, and hemolytic procedure.
|
Services
Why Choose Us?
Choosing Creative Biolabs means partnering with a leader in Complement System Therapeutic research for Acute Ischemic Stroke. With over 20 years of specialized experience, our team offers unparalleled scientific knowledge and a deep understanding of complement biology, committed to accelerating your drug discovery.
Our key advantages include:
-
Unrivaled Expertise: Extensive experience ensures cutting-edge insights and robust experimental design.
-
Comprehensive Platform: Integrated services from target ID to preclinical support provide seamless workflow.
-
High-Quality Reagents and Products: We provide pure, functional proteins, antibodies, and assay kits for reliable results.
-
Customized Solutions: Services are highly customizable to meet unique project objectives.
-
Rapid Turnaround Times: Efficient processes ensure timely delivery, meeting critical project timelines.
-
Proven Track Record: Our commitment to scientific excellence is reflected in successful collaborations and quality outputs. (Published Data)
Obtain the Creative Biolabs Advantage - Request Details Immediately
FAQs
Q: How does complement inhibition specifically target stroke damage without compromising essential immune functions?
A: The goal of complement inhibition in stroke is to selectively block the detrimental aspects of complement activation that contribute to secondary brain injury, while ideally preserving its vital roles in host defense. This often involves targeting specific components or pathways that are predominantly involved in pathological inflammation rather than general immunity, or using strategies that transiently inhibit complement during the acute phase of injury. Research focuses on identifying the most appropriate targets and therapeutic windows to achieve this balance.
Q: What are the key considerations when developing complement-targeting therapeutics for neurological conditions?
A: Developing therapeutics for neurological conditions requires careful consideration of several factors. These include the ability of the therapeutic agent to cross the blood-brain barrier, its specificity for the intended complement target, potential off-target effects, and the optimal timing and duration of administration to maximize neuroprotection while minimizing systemic side effects. Understanding the precise mechanisms of complement activation in the specific neurological context is also crucial.
Q: Can complement modulation strategies be combined with existing stroke treatments?
A: Yes, there is significant interest in exploring combination therapies. Complement modulation strategies could potentially be used as an adjunct to standard reperfusion therapies, such as thrombolysis or thrombectomy, to further reduce ischemia-reperfusion injury. The aim would be to provide additional neuroprotection and improve overall outcomes by mitigating the inflammatory and damaging effects of complement activation that persist even after blood flow is restored.
Q: What are the potential challenges in translating complement-based therapies from preclinical studies to clinical applications?
A: Translational challenges for complement-based therapies often include demonstrating consistent efficacy across diverse patient populations, determining optimal dosing and administration routes, managing potential systemic side effects associated with broad complement inhibition, and navigating the complexities of clinical trial design for acute neurological conditions. Identifying reliable biomarkers for complement activation and therapeutic response in patients is also a key hurdle.
Q: How can researchers assess the efficacy of complement inhibitors in in vitro or in vivo stroke models?
A: Efficacy assessment in stroke models typically involves a multi-faceted approach. In vitro, researchers can use neuronal cell cultures exposed to ischemic conditions to measure cell viability, apoptosis, and inflammatory marker expression in the presence of inhibitors. In vivo, animal models of ischemic stroke allow for the evaluation of infarct volume reduction, neurological deficit scores, brain edema, blood-brain barrier integrity, and the quantification of complement component deposition in brain tissue.
Creative Biolabs is at the forefront of Complement System Therapeutic research, offering unparalleled expertise and a comprehensive suite of products and services to advance your understanding and development of treatments for acute ischemic stroke. Our commitment to scientific excellence and customized solutions ensures that your project receives the highest level of support.
Featured Services
Feature Products
Reference
-
Alawieh, Ali et al. "Complement in the Homeostatic and Ischemic Brain." Frontiers in immunology vol. 6 417. 12 Aug. 2015, DOI:10.3389/fimmu.2015.00417. Distributed under an Open Access license CC BY 4.0, without modification.
For Research Use Only.
Related Sections:

 Fig.1 Schematic diagram of the triggers of complement activation after cerebral ischemia-reperfusion injury.1
Fig.1 Schematic diagram of the triggers of complement activation after cerebral ischemia-reperfusion injury.1