Introduction What We Can Offer? Why Choose Us? FAQs Featured Services Featured Products
Accelerate Your Research and Development!
Are you currently facing challenges in developing effective treatments for ocular inflammatory diseases, particularly anterior uveitis, or struggling with long drug development cycles for targeted therapies? Creative Biolabs' Complement System Therapeutic solutions help you accelerate the discovery and development of novel interventions for anterior uveitis, enabling the obtainment of high-quality research tools and the development of highly specific therapeutics through advanced complement system modulation techniques and comprehensive service platforms.
Contact our team to get an inquiry now!
Introduction
Anterior uveitis is a prevalent form of intraocular inflammation affecting the iris and ciliary body, characterized by symptoms such as eye pain, redness, photophobia, and blurred vision. Its etiology is diverse, ranging from autoimmune conditions and infections to trauma, often leading to significant visual impairment if left untreated. While traditional treatments primarily involve corticosteroids and dilating drops to manage inflammation, a deeper understanding of the underlying immunological mechanisms is crucial for developing more targeted and effective therapies.
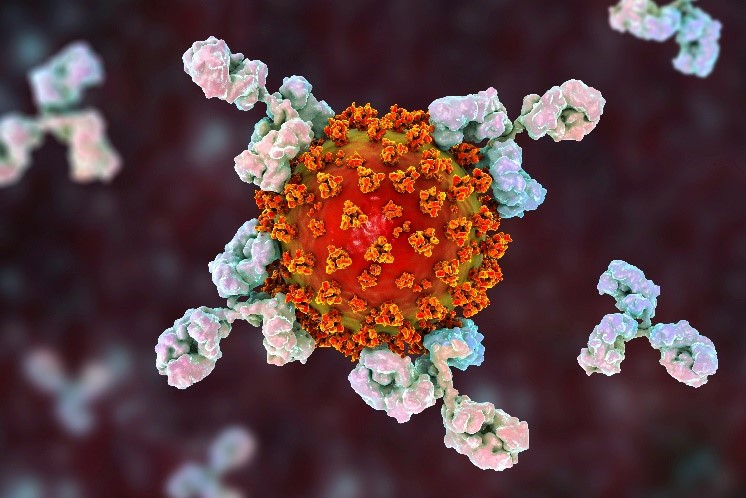
The complement cascade, an essential constituent of innate immunity, fulfills pivotal but intricate functions in ophthalmic well-being and pathology. This elaborate sequence of plasma proteins proves indispensable for defending against pathogens and eliminating antigen-antibody aggregates plus dying cells. Yet complement malfunction may provoke unchecked inflammation and cellular harm, driving disease progression in diverse inflammatory disorders, including ophthalmic conditions. Studies confirm complement operates as a dual-function mechanism in eye-related contexts; protective during homeostasis, its abnormal triggering can intensify inflammation in disorders such as uveitis.
Complement System in Anterior Uveitis
Studies have demonstrated the presence of complement components within the inflamed eyes of uveitis patients, highlighting their active involvement in the inflammatory process. Specifically, anaphylatoxins such as C3a and C5a, potent inflammatory mediators generated during complement activation, contribute significantly to the recruitment of immune cells and the perpetuation of inflammation within the uvea. The classical, alternative, and lectin pathways of complement activation have all been implicated in ocular inflammatory diseases, with various complement components (e.g., C1q, C3, C4, C5, Factor B, Factor D, properdin) and regulators (e.g., Factor H, CD59, DAF) found in ocular tissues. Consequently, modulating specific components of the complement system represents a promising therapeutic strategy for mitigating inflammation and preventing ocular damage in anterior uveitis, offering a targeted approach beyond general anti-inflammatory interventions.
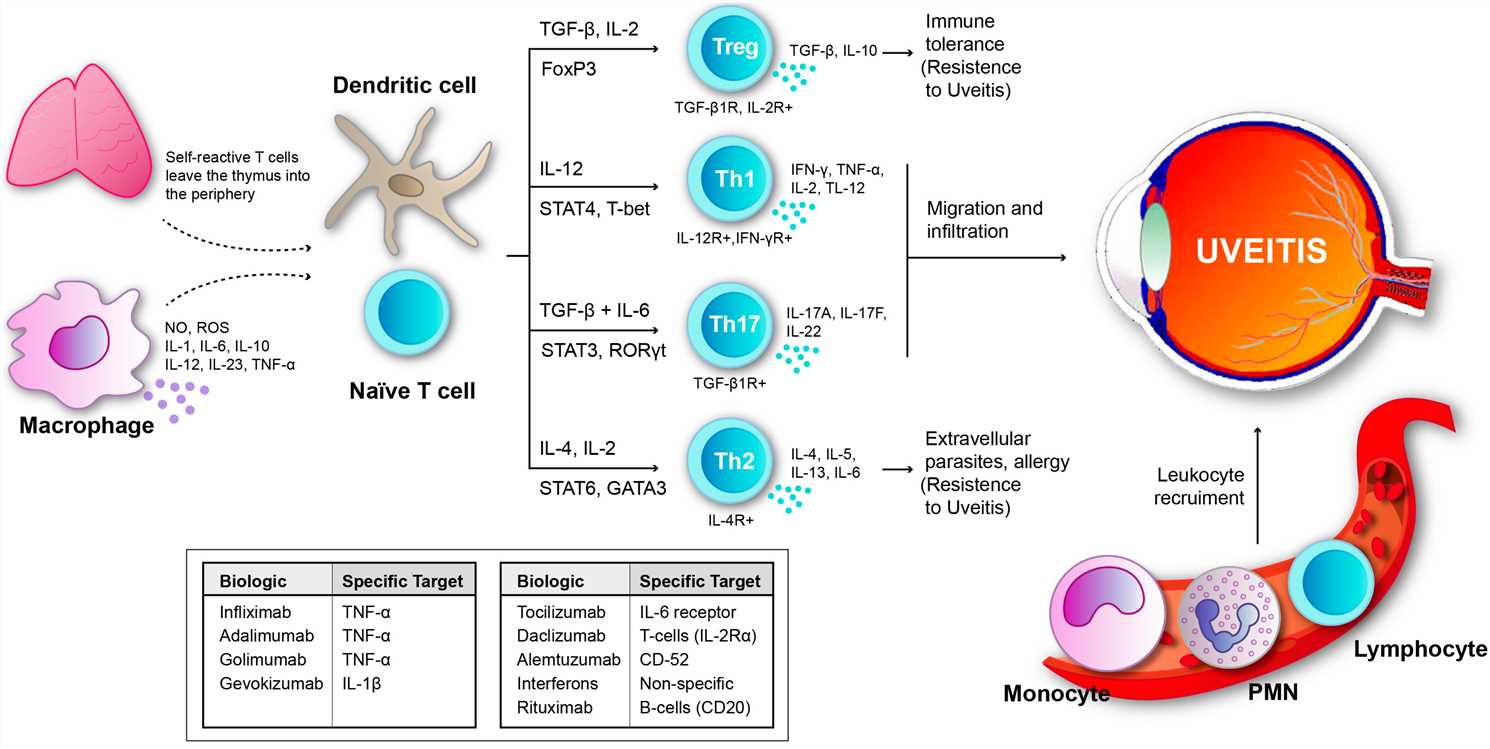 Fig.1 Uveitis results from an imbalance between inflammatory mechanisms and regulatory mechanisms.1
Fig.1 Uveitis results from an imbalance between inflammatory mechanisms and regulatory mechanisms.1
What We Can Offer?
Creative Biolabs provides a comprehensive suite of products and services designed to facilitate research and therapeutic development targeting the complement system in anterior uveitis:
Complement-Related Products
-
High-quality recombinant complement proteins (e.g., C3, C5, Factor B, Factor D, MASP-2, C1s).
-
Specific antibodies targeting various complement components and regulators for research and therapeutic applications.
-
Complement activity assay kits for measuring pathway-specific activation (classical, alternative, lectin pathways).
Complement-Related Services
-
Custom Antibody Development: Development of highly specific monoclonal and polyclonal antibodies against complement targets, including inhibitory and neutralizing antibodies.
-
Complement Activity and Inhibition Assays: Comprehensive assays to quantify complement activation, assess the inhibitory potential of novel compounds, and evaluate complement-mediated cytotoxicity.
Why Choose Us?
Choosing Creative Biolabs for your Complement System Therapeutic research in anterior uveitis means partnering with a leader in ocular immunology and therapeutic development. Our unparalleled expertise, combined with state-of-the-art platforms, positions us to deliver exceptional results for your project.
-
Cutting-Edge Technology: We leverage advanced recombinant DNA technology, high-throughput screening platforms, and innovative protein engineering techniques to identify, develop, and optimize novel complement modulators.
-
Comprehensive Service Portfolio: From target validation and lead discovery to preclinical development, our integrated services cover every stage of therapeutic development, ensuring a seamless and efficient workflow.
-
Rigorous Quality Control: Every project at Creative Biolabs adheres to stringent quality control standards, guaranteeing the reliability, reproducibility, and high quality of all deliverables, from reagents to therapeutic candidates.
-
Client-Centric Approach: We prioritize understanding your specific project needs and objectives, offering customized solutions and dedicated scientific support to ensure your research goals are met with precision and efficiency.
-
Proven Track Record: Our success stories and Published Data demonstrate our capability to deliver impactful solutions in complex therapeutic areas, including complement-mediated diseases.
You can gain an edge with Creative Biolabs – Inquire right away
FAQs
Here are some common questions from researchers and developers exploring complement-targeted therapies for ocular inflammation:
Q: How does complement system modulation specifically enhance anterior uveitis therapy?
A: Regulating complement activity provides a targeted strategy to disrupt pathological inflammatory pathways in anterior uveitis. Selective inhibition of key complement elements suppresses inflammatory signaling molecules such as C3a/C5a, curbing leukocyte migration and preserving ocular tissue integrity, ultimately enhancing visual prognosis and lowering relapse rates.
Q: What types of therapeutic modalities are typically considered when developing complement-targeted interventions for ocular diseases?
A: A range of therapeutic modalities can be developed. These include monoclonal antibodies designed to neutralize specific complement proteins, small molecule inhibitors that block enzymatic activities within the cascade, and even gene therapies aimed at regulating complement protein expression. The determination typically relies upon the particular therapeutic target and intended intervention mode.
Q: What are the key advantages of focusing on complement modulation for ocular inflammatory conditions compared to broader anti-inflammatory treatments?
A: The primary advantage lies in specificity. While general anti-inflammatory drugs can suppress overall immune responses, complement modulation allows for a more targeted intervention at a crucial point in the inflammatory cascade. This can lead to more potent effects on the specific disease pathway while potentially minimizing systemic side effects associated with broad immunosuppression.
Q: Are there any particular challenges or precautions to consider when developing therapies that target the complement system for ophthalmic applications?
A: Yes, challenges include ensuring effective drug delivery to the eye, minimizing potential off-target effects on the protective functions of the complement system, and managing the risk of unwanted immune responses against the therapeutic agent. Meticulous planning and thorough validation prove imperative to surmount obstacles.
Q: How can researchers determine if complement dysregulation is a significant factor in their specific model of anterior uveitis or in patient samples?
A: Researchers can assess complement involvement through various methods, including measuring levels of activated complement components (e.g., C3a, C5a, sC5b-9) in ocular fluids (aqueous humor, vitreous) or serum. Additionally, immunohistochemical staining of ocular tissues for complement deposits and genetic analyses for complement regulatory protein polymorphisms can provide valuable insights.
Creative Biolabs is your trusted partner for advancing research and developing therapeutic solutions focused on the complement system in anterior uveitis. Our comprehensive offerings, from high-quality reagents to advanced research services, are designed to accelerate your project and bring innovative treatments closer to patients.
Featured Services
Feature Products
Reference
-
Mérida, Salvador et al. "New Immunosuppressive Therapies in Uveitis Treatment." International Journal of Molecular Sciences vol. 16,8 18778-95. 11 Aug. 2015, DOI:10.3390/ijms160818778. Distributed under an Open Access license CC BY 4.0, without modification.
For Research Use Only.
Related Sections:

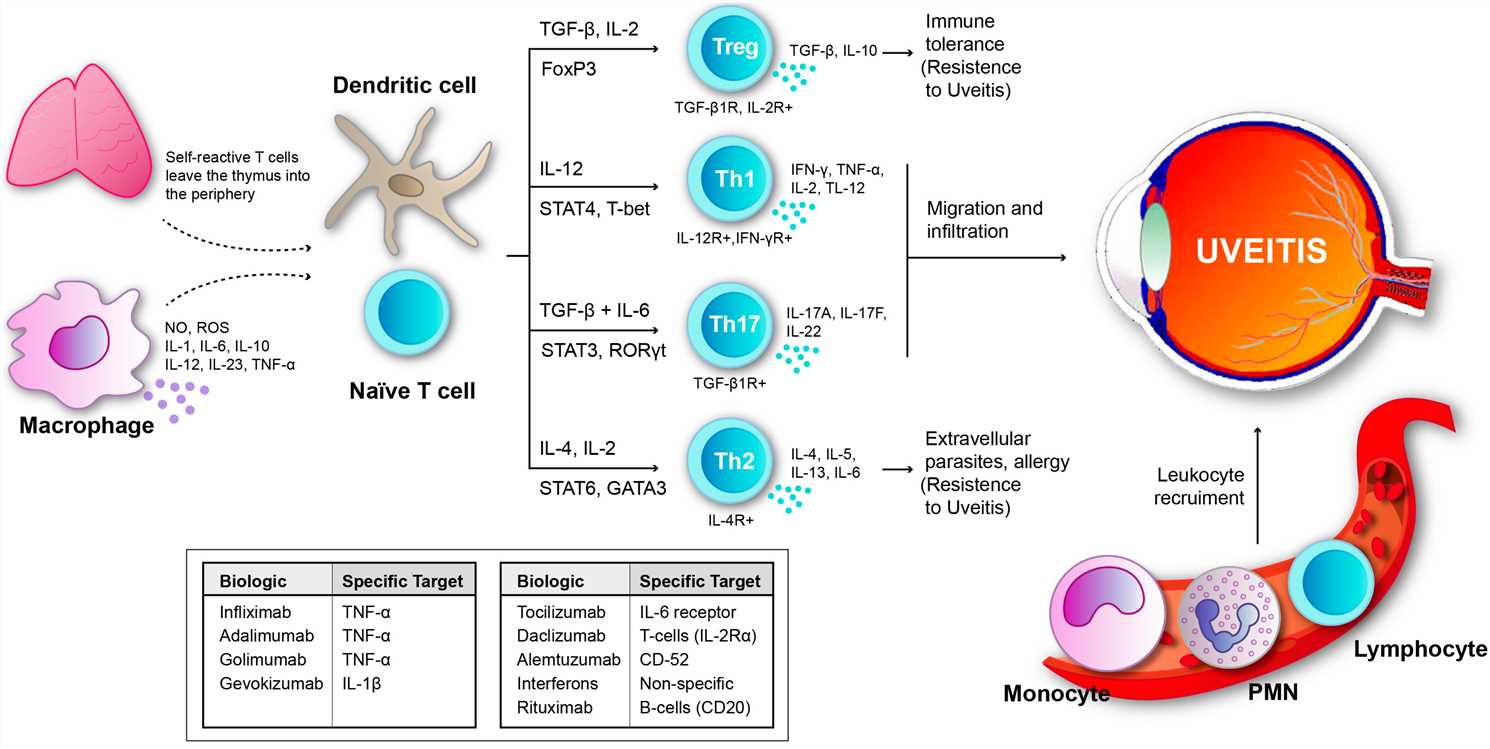 Fig.1 Uveitis results from an imbalance between inflammatory mechanisms and regulatory mechanisms.1
Fig.1 Uveitis results from an imbalance between inflammatory mechanisms and regulatory mechanisms.1