Candida auris
Infections by pathogenic fungi have emerged as an increasingly significant problem in human health. However, the effects of fungi infection are not widely recognized and mortality rate caused by such infections has usually been ignored. Recently, candidiasis, especially those caused by infection with non-albicans Candida spp., has attracted great attention. As always focus on the research spotlight of drug discovery, Creative Biolabs is now proud to offer a series of antifungal drug discovery services against C. auris.
Introduction to Candida Auris
Candida auris (C. auris) is a species of ascomycetous fungus which typically grows as yeast. It belongs to the Candida spp. and forms smooth, whitish-gray, shiny, viscous colonies on growth media. These yeast cells are microscopically ellipsoid in shape. C. auris is identified as one of the few species of this genus that can cause candidiasis in humans. Candidiasis is usually infected by immunocompromised patients in the hospital environment. C. auris can cause invasive candidiasis that the bloodstream, the central nervous system (CNS), and internal organs (such as kidneys, liver, spleen, bones, joints, muscles, or eyes) are infected. Patients can remain infected with C. auris for a relatively long time, while C. auris can persist on the surface of healthcare facilities.
Pathogenesis of C. Auris
The ability of Candida species to cause infection is due to the possession of various virulence factors, such as adhere to host cells, the ability to germinate, biofilm formation, and the secretion of extracellular enzymes including proteinase and phospholipase. C. auris strains have reported showing significantly diminished ability to adhere to catheter material when compared with C. albicans. Datas also indicated that C. auris produces phospholipase and proteinase in a strain-dependent manner. Unlike C. albicans, C. auris biofilms possess a limited number of the extracellular matrix. What’s more, the biofilm thickness of C. auris was significantly less than that of C. albicans.
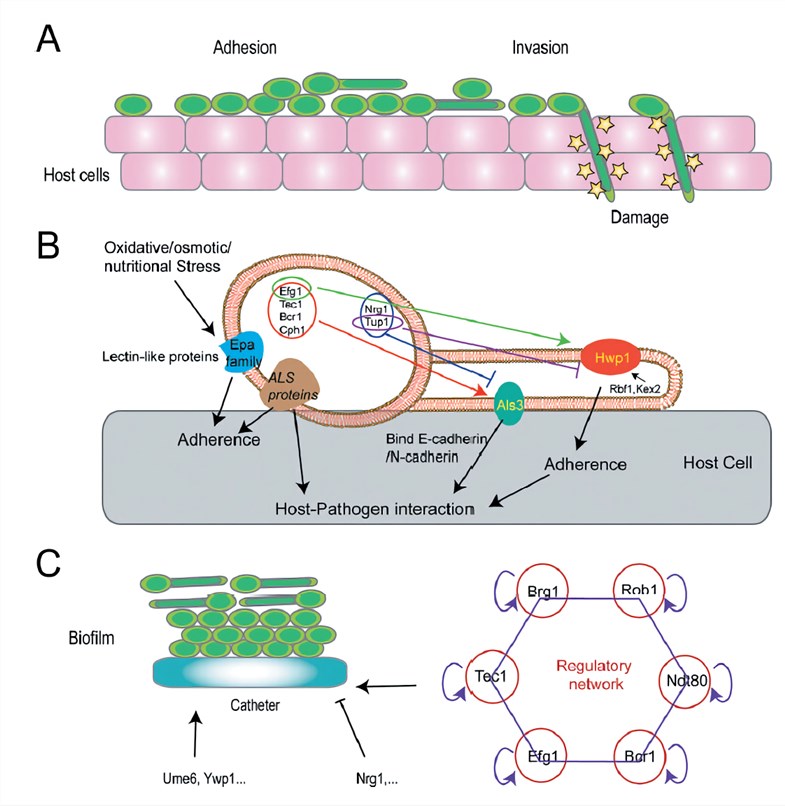 Fig.1 An overview of fungal pathogenicity mechanisms.1
Fig.1 An overview of fungal pathogenicity mechanisms.1
Antifungal Drugs Against C. Auris
Generally speaking, the anti-fungal drugs now available can be classified into the five categories as follows: azoles, ployenes, allylamines, echinocandins, and flucytosine. Treatment of C. Auris is considered complicated because it is easily misidentified as other Candida species. Most of the C. auris infections are treatable with antifungal drugs known as echinocandins. However, C. Auris has recently aroused significantly increased attention due to its multidrug resistance. Some C. auris infections have proved to be resistant to the major types of antifungal agents. Under this condition, multiple antifungal drugs at high doses may be required to treat the C. auris infection.
Antifungal Drug Discovery Services Against C. Auris at Creative Biolabs
Over the last decades, the importance of antifungal drugs in the practice of modern medicine has increased significantly. Creative Biolabs is recognized as a world leading CRO who is focused on the field of antifungal drug discovery. Our scientists devote themselves to delivering the highest quality, full-service contract research especially for antifungal drug discovery services, including target identification and validation, Hit identification, Hit to lead, Lead optimization, and IND enabling.
You may also be interested in other fungi that may be implicated in candidiasis:
If you are interested in our antifungal drug discovery services, please do not hesitate to contact us for more details.
Reference
- Gao, N.; Chen, C. Candida Infections: An Update on Host Immune Defenses and Anti-Fungal Drugs. Infectious Diseases and Translational Medicine. 2016, 2(1), pp.30-40. Distributed under Open Access license CC BY 4.0, without modification.
For Research Use Only.
