The United States FDA approved the extended indication of its antibody coupling drug Kadcyla (ado-trastuzumab emtansine) as a postoperative adjunctive therapy for early mammary cancer patients with positive HER2 and still residual lesions after receiving neoadjuvant therapy. The approval of this treatment not only provides a new treatment option for patients with early mammary cancer but also validates a new model of clinical trials for patients with early high-risk breast cancer.
Breast cancer is one of the most common cancers among women in the world. According to the American Cancer Society, there were about 271000 new breast cancer patients in the United States in 2019, and 42000 patients will die of breast cancer. About 15% to 20% of a range of different types of breast cancer are HER2-positive. The cancer cells of these patients express HER2 protein on the surface.
Introduction to Kadcyla
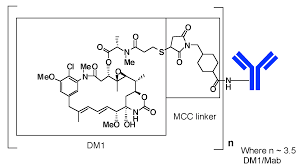
For these patients, targeted HER2 therapy is expected to bring good results. Kadcyla is one of many treatments. As an antibody-drug conjugate, its antibody partial trastuzumab, the main active component of Herceptin, targets HER2. Another part of it is the chemotherapeutic drug DM1. The drug is supposed to bind to cancer cells that express HER2 and kill them. At present, Kadcyla is the only antibody-drug conjugate approved in the United States to treat HER2 positive early mammary cancer and metastatic breast cancer.
The efficacy of Kadcyla was validated in phase 3 clinical trial called KATHERINE. Compared with the group of patients who used Herceptin, the risk of breast cancer recurrence or all-cause death decreased significantly by 50% in the group of patients who used Kadcyla (HR=0.50,95% CI: 0.39 0.64 p / Ltd 0.0001). At the 3-year node, 88.3% of patients treated with Kadcyla had no recurrence of breast cancer compared with 77.0% in the control group.
FDA approval of Kadcyla
It is worth mentioning that in order to speed up the drug development and evaluation process, the drug clinical trial design and evaluation process use a variety of acceleration channels provided by the FDA. In the design of clinical trials, the researchers used the alternative endpoint of Pathological Complete Response (pCR) introduced by the FDA as a criterion to screen patients with early mammary cancer who had received neoadjuvant therapy. According to FDA’s guidelines, pCR is defined as that after the completion of neoadjuvant therapy, there are no residual invasive (and in situ) tumors in the resected breast and in the surrounding lymph nodes. In KATHERINE clinical trials, only patients who did not reach pCR after neoadjuvant therapy were included in the next clinical trial and received adjuvant therapy with Kadcyla or Herceptin.
This clinical trial design for patients with high-risk early mammary cancer can not only complete patient registration earlier, but may also lead to earlier results. Dr. Richard Pazdur, director of the Center for Excellence in Oncology at FDA and acting director of the Office of Hematology and Oncology Products at the FDA Center for Drug Evaluation and Research, commented in the New England Journal of Medicine. This paper expounds the advantages of this clinical trial design in speeding up the development of new drugs for breast cancer and benefiting high-risk early patients.
The drug was approved through the FDA’s Real-Time Oncology Review (RTOR) and Assessment Aid pilot program, which allowed the treatment to be approved just 12 weeks after the application was submitted. With the approval of the drug, early mammary cancer patients are expected to have new treatment options, which can also give them the best hope of a cure. “This approval is of great significance for the treatment of HER2-positive early mammary cancer. By working closely with FDA in the United States and participating in the RTOR pilot project, we brought Kadcyla to patients with residual lesions after neoadjuvant therapy in a much shorter period of time than expected.” Dr. Sandra Horning, Chief Medical Officer and head of Global Product Development at Genentech, said: “By reducing the risk of recurrence, we are closer to the goal of maximizing the hope of a cure for every patient with early mammary cancer.”