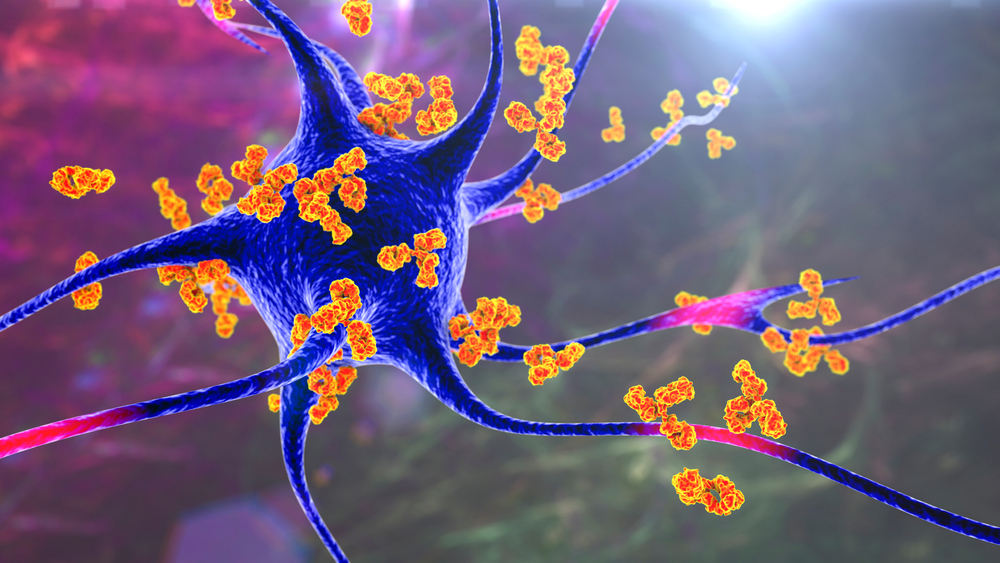
An autoimmune disease is a pathological condition resulting from an abnormal immune response to tissues that can exist in the body, affecting up to 50 million Americans in terms of the American Autoimmune Related Diseases Association (AARDA). There are as many as 80 types of Autoimmune diseases, most of which have like symptoms, making it very difficult to diagnose. Autoimmune diseases can affect almost any part of the body, including the heart, brain, nerves, muscles, skin, eyes, joints, lungs, kidneys, glands, The digestive tract, and blood vessels.
Researchers have found that a method will remove certain B cells that produce antibodies and lead to autoimmune diseases without damaging the rest of the immune system.The key to this new treatment strategy is CAR, the artificial receptors that identify target cells, which will be expressed in T cells of patients body with gene modification. In human clinical trials, scientists extracted a number of T cells from a patient through a dialysis-like process, and then genetically modified them in the laboratory to introduce genes that encode CARs so that these T cells were able to express this new receptor. These genetically modified T cells proliferated in the laboratory and then were transfused into the patient body. These T cells bind to the surface of the target cell using the CAR receptors they express, and this binding triggers an internal signal to activate T cells for rapidly destroying the target cell.
A blastoma refers to the tumor that arises from embryonic tissue, typical use childhood cancer. The term blastoma is generally included as part of the full medical name of a specific tumor, as in medulloblastoma, neuroblastoma, or pleuropul blast blastoma.
Immunotherapy of adoptive T cells provides a very promising treatment for specific targeted therapies and the eradication of malignant gliomas. T cells are capable of processing and expressing chimeric antigen receptors in vitro that target glioblastoma antigens. The proliferation and function of adoptive T cells can be enhanced by lymphodepletive and standard tumor necrosis caused by standard radiotherapy and chemotherapy. A CAR-T cell produces EGFRvIII (a glioblastoma surface antigen) that evaluates its effect in the standard care of the glioblastoma mouse model. T cells were processed by lentiviral vector transduction of a CAR gene that targets EGFRvIII. The tumor animal model uses a series of temozolomide and clinical-level dose of whole brain radiation therapy, and then transfuse into the animal body through intravenous injections. This method can be used to assess the anti-tumor ability of CAR-T cell technology under the standard care.
CAR-T cell therapy technology shows the most promising development trend in a variety of cell therapy strategies.The success of CAR-T has brought the dawn of victory to the campaign against these incurable diseases. As a biological therapy with the most rapid development, CAR-T therapy has attracted a great attention from scientific research institutions across the world. But in fact, CAR-T cell technology is also facing a lot of problems which will not only affect the development prospects of CAR-T cell therapy technology but also determines the treatment effect. In order to obtain more effective CAR-T, it is necessary to further improve the specificity of CAR-T target, promote the migration of CAR-T cells, and control the time of cell amplification.