1. RNA vaccine
RNA-based vaccines have great potential as a way to treat cancer or prevent a variety of infectious diseases. As a result, many biotechnology companies are now developing this type of vaccine, and some are already in clinical trials. One of the challenges of making RNA vaccines is to ensure that RNA enters the right immune cells and produces enough proteins. In addition, the vaccine must trigger a strong enough immune response so that the immune system can destroy the associated bacteria, viruses, or cancer cells when they subsequently encounter them.
Now, scientists at the Massachusetts Institute of Technology have developed a new series of lipid nanoparticles to deliver the vaccine. They have shown that these particles promote the expression of proteins encoded by RNA, and additionally, similar to adjuvants, they further improve the efficacy of the vaccine. In the study of mice, they used the RNA vaccine to successfully inhibit the growth of melanoma tumors.
“One of the main findings of this paper is that you can build RNA vectors that activate the immune system efficiently,” said Daniel Anderson, an associate professor of chemical engineering at MIT and a member of the Koch Institute of MIT. The study was published in the Sept. 30 issue of the journal Nature Biotechnology.
Most traditional vaccines are made from pathogen-related proteins or attenuated microbes. In recent years, scientists have explored to make vaccines through DNA, which encodes microbial proteins. However, these vaccines have so far failed to produce a strong enough immune response and have not yet been approved for use in humans.
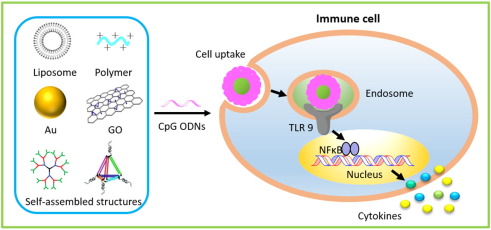
Unlike DNA, which must reach the nucleus to function, RNA can be translated into protein as soon as it enters the cytoplasm. So it can also be applied to many different diseases. “Another advantage of these vaccines is that the targets are very flexible. We can quickly prepare vaccines for different diseases by repairing RNA sequences.” RNA vaccine needs to enter an immune cell called an antigen-presenting cell to be more effective, and it will produce a protein encoded by the vaccine and display it on its surface, attracting and activating T cells and other immune cells.
2. Lipid nanoparticles delivery system Experiment
Anderson’s laboratory has previously developed lipid nanoparticles for the delivery of RNA and DNA molecules. These lipid particles form tiny droplets that protect RNA molecules and take them to their destination. The usual approach is to generate a library of hundreds of candidate particles with different chemical characteristics and then screen them to find the best part. “In one day, we can synthesize more than 1000 lipid materials with a variety of different structures. Once we have a very large library, we can screen molecules and see what types of structures can help RNA transfer to antigen-presenting cells. “
They found that nanoparticles with a circular structure at one end of the particles can trigger the immune signaling pathway of STING. Once the pathway is activated, the cells will produce interferons and other cytokines, activating T cells.
The researchers tested the effects of these particles in two different melanoma mouse models. First, they made a test in genetically modified mice that could express ovalbumin. The researchers designed an RNA vaccine against ovalbumin and showed that the vaccine prevented tumor growth and significantly prolonged the survival of mice. Then, the researchers produced a vaccine against Trp2, a protein naturally produced by melanoma tumors. The vaccine also stimulated a strong immune response, slowing tumor growth and improving the survival rate of mice.
