On February 1, NEJM, the top medical journal, published the results of a pivotal multi-center critical phase 2 trial in support of the “first CAR-T therapy Tisagenlecleucel listed”. The overall survival of patients reached 76% after 12 months of treatment, and CAR-T cells remain in the patient for up to 20 months. Daniel June is the co-author of the paper.
Just nine months ago, the U.S. FDA approved Tisagenlecleucel for the treatment of acute lymphoblastic leukemia (ALL) in children and young adults. This is the first listing CAR-T therapy worldwide, opening up a new era in the treatment of childhood leukemia.
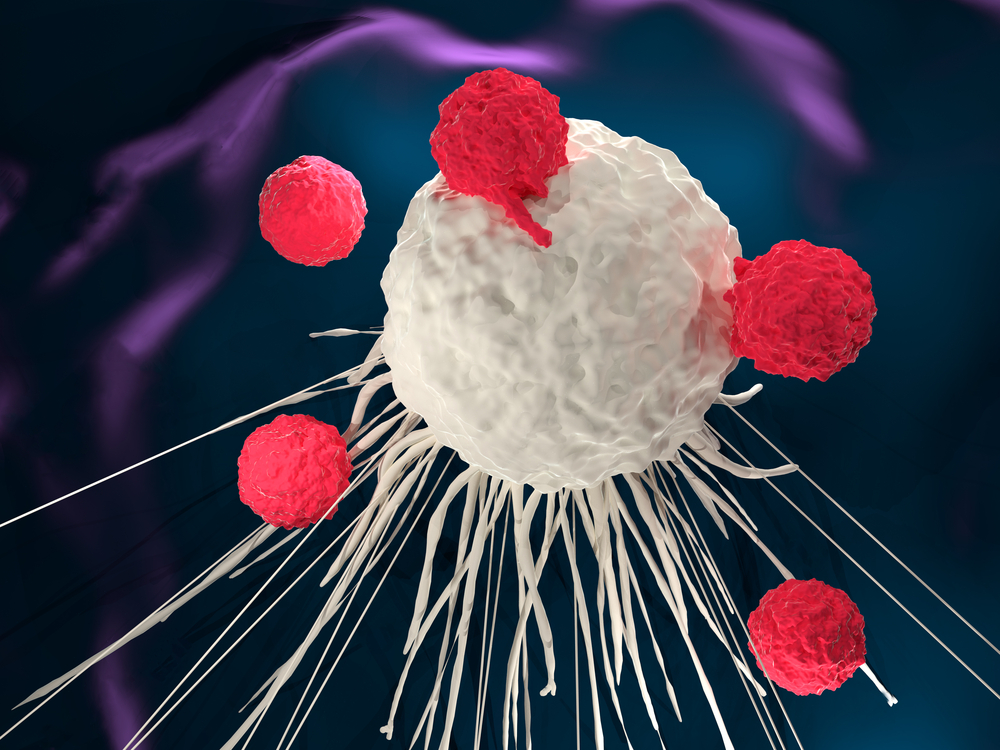
In simple terms, CAR-T therapy involves the isolation of T cells from a patient and the modification of T cells in vitro with a “navigation”, chimeric antigen receptor (CAR) that specifically targets cancer cells. Then these “modified CAR-T cells” were amplified and returned to the patient’s body to play a specific anti-cancer effect.
In fact, the therapy was first developed by a team led by Carl June, Ph.D., Perelman School of Medicine, University of Pennsylvania. The June team then partnered with Philadelphia Children’s Hospital, the first institution to use CAR-T to treat childhood leukemia. Dr. Stephan A. Grupp from the hospital and Dr. Michael A. Pulsipher from Los Angeles Children’s Hospital are the senior authors in this new paper
1. CAR-T cells are maintained in the patient for 20 months
Specifically, the new study reports the latest data from the ELIANA trial in 25 centers in 11 countries around the world (a long-term follow-up of the safety and efficacy of CAR-T treatment). The 75 patients involved were between 3 and 21 years of age with recurrent or refractory B-cell ALL. 61% of the patients relapsed after receiving allogeneic hematopoietic stem cell transplantation.
The analysis showed that the overall remission rate of 75 patients was 81% (that is 61 patients responded to CAR-T therapy) at 3 months of treatment. The recurrence rate of the 61 patients was 80% after 6 months of treatment. At the 12th month, it reached 59%. In addition, the overall survival for all 75 patients was 90% at the 6th month and 76% at the 12th month.
With a sustained response, CAR-T cells were maintained in the patient for up to 20 months with a median persistence of 168 days. At the same time, it is worth mentioning that all patients in the trial received only a single injection of CAR-T cells.
In terms of safety, CAR-T treatment also has a lot of side effects, which is consistent with earlier studies. In the study, 73% of patients developed grade 3 or 4 adverse events that may be associated with the therapy. Among them, the most serious side effects include cytokine release syndrome and neurotoxicity events. However, most side effects are transient and reversible.
2. CAR-T therapy is feasible in many regions of the world
Dr. Shannon L. Maude, the lead author of the paper, said that this expanded global study further demonstrates the potential of CAR-T for the treatment of young ALL patients. Our data show that CAR-T therapy can make patients get more long-term remission and survival while these personalized cancer cells can maintain in the body with months, or even years, and effectively play the role.
Dr. Pulsipher said: “There were not many other things we could do for patients who had recurrent or nonresponsive treatment after transplantation, but now CAR-T therapy has changed that.” In this study, we work with a number of people to demonstrate that CAR-T therapy is not only feasible in many parts of the world but also equally safe and effective.
It is reported that the scientists are conducting further clinical trials to investigate ways to reduce serious side effects and to overcome recurrence. We hope that with the concerted efforts of global scientists, this new type of anti-cancer therapy will save more lives.
References:
1) Study: CAR T-cell therapy safe and effective in youth with leukemia
2) T Cell Therapy Shows Persistent Benefits in Young Leukemia Patients