Huge progress has been made in the CAR-T field recently. Professor Koji Tamada from Yamaguchi University, Department of Immunology, has successfully developed a new generation of CAR-T.
Meanwhile, in a variety of solid tumor mouse models, Professor Tamada confirmed that this new CAR-T cell therapy induced complete regression of tumor, which led to long-term survival of the mice without tumor recurrence and with at least 4 times superior anti-tumor activity compared to conventional CAR-T cells. And even 100 days after the new generation of CAR-T eliminated solid tumors, tumors cell could not grow when they were inoculated again. The discovery was published in the Nature Biotechnology.
So, what has changed of the new generation of CAR-T? To answer this question, we need to understand CAR-T therapy simply. The goal of CAR-T is nothing more than a transformation of common T cells to give it a stronger ability to fight tumors more accurately and effectively [2]. It’s like that the bravest soldier can’t defeat the evil alone without his teammates. Many hands make light work, wood flame high. This is the most important change in the new generation of CAR-T, from simply killing cancer cells to being able to carry immune regulators to assemble immune cells to fight together.
Prof. Tamada’s research group has long been committed to the transformation and optimization of CAR-T in an effort to apply CAR-T to solid tumors. Previous studies have revealed that IL-7 and CCL19 produced by T-zone fibroblastic reticular cells are essential for the formation and maintenance of the T-cell zone in lymphoid organs, where both T cells and DCs are recruited from the periphery by CCL19. IL7 can promote T cell proliferation while maintaining the stability of T cells. This brought Professor Tamada hope. The new generation of CAR-T developed by Professor Tamada is actually transformed on the basis of the conventional CAR-T, so that the conventional CAR-T can express two chemokines IL7 and CCL19. Therefore, the new generation CAR-T is also named 7 × 19 CAR-T.
Obviously, Professor Tamada believed that if CAR-T can express IL7 and CCL19, the new generation CAR-T that enters solid tumors can imitate T-zone fibroblastic reticular cells in lymphoid tissue and assemble immune cells from other parts to fights against solid tumors. In in vitro experiments, Professor Tamada found that the new generation CAR-T expressing IL7 and CCR19 has twice the capacity of proliferation and at least 5 times the ability to recruit immune cells in transwell migration assays that of conventional CAR-T treatment. At the same time, IL7 receptor inhibitors can completely eliminate the enhanced proliferative capacity of the new generation CAR-T, and CCL19 receptor inhibitors can also completely eliminate the ability of the new generation of CAR-T to recruit immune cells. These experiments show that the proliferative capacity of the new generation CAR-T and the ability to recruit immune cells are indeed conferred by IL7 and CCR19. Compared to conventional CAR-T (Figure 1. white), the ability of the new generation CAR-T (Figure 1. red) to recruit immune cells is significantly enhanced.
Subsequently, Professor Tamada began testing the in vivo anti-tumor activity of the new generation CAR-T. Normal CAR-T or a new generation CAR-T treatment were accepted in mice treated with moderate cyclophosphamide pretreatment. Results showed that conventional CAR-T can only slightly improve the survival of mice with mast cell tumors, while the new generation of CAR-T can completely eliminate the tumors of all experimental mice without recurrence within the 140-day observation period.
Interestingly, Professor Tamada also proved that a single injection of 1×10^6 new generation CAR-T cells resulted in better anti-tumor effects than injection of 4×10^6 conventional CAR-T cells. In other words, the anti-tumor effect of the new generation of CAR-T cells is at least 4 times that of conventional CAR-T.
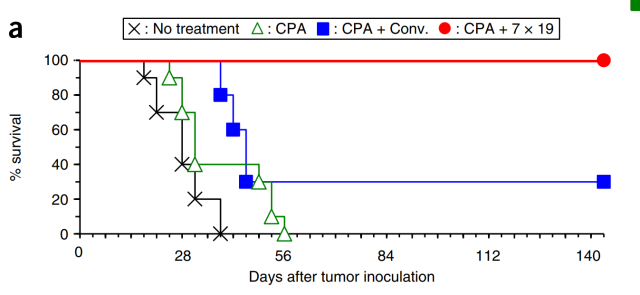
Figure 2. The survival rate of mice with red and blue representing the new generation and the conventional one
Later, Professor Tamada also conducted in vivo anti-tumor experiments using a murine pancreatic ductal adenocarcinoma It was found that although conventional CAR-T is essentially ineffective for lung adenocarcinoma and completely ineffective for pancreatic cancer while the new generation of CAR-T also achieves complete elimination of tumor tissue in mice with lung adenocarcinoma, and suppressed the tumor growth and prolonged mouse survival in mice with pancreatic cancer. At the same time, in order to examine whether simultaneous expression of IL-7 and CCL19 are essential for the therapeutic effects of 7 × 19 CAR-T cells, Professor Tamada designed CAR-T expressing ether IL-7 or CCL19 alone. As expected either 7CAR-T or 19CAR-T, or even 1:1 mixture of the two, was only comparable to the normal CAR-T effect, suggesting that the concomitant production of IL-7 and CCL19 from individual CAR-T cells is necessary to induce the anti-tumor potential of 7 × 19 CAR-T cells.
In addition, through imaging and tissue biopsy in live mice, Professor Tamada found that the new generation of CAR-T rather than conventional CAR-T, can all enter solid tumors after injection, and induced a large number of body’s own T cells and dendritic cells into solid tumor tissue to exert their anti-cancer effects.
Finally, Professor Tamada also found that mice receiving 7 × 19 CAR-T treatment have a large number of cancer memory T cells in their bodies, which can effectively prevent cancer recurrence. Overall, Professor Tamada has successfully developed a new generation of CAR-T that can effectively fight solid tumors, meaning that appropriate combination of CAR and immune regulatory factors such as IL17 and CCR19, etc., can effectively enhance the anti-solid tumor activity of CAR-T and the body’s own T cells.
As Professor Tamada said, “Our research shows that CAR-T cells can not only directly exert their anti-cancer effects, but also serve as cell vectors to deliver immunomodulatory molecules to the tumor microenvironment, thereby in vivo triggering, enhancing and maintaining anti-tumor immune response.” At present, Professor Tamada’s team is discussing clinical cooperation with Noiruimyun Biotech.
Creative Biolabs CellRapeutics as a world-renowned service provider for immunotherapy, have one of the world’s largest collection of CAR products of different generations targeting various biomarkers, and we continue to innovate the next generation CAR technologies to achieve even greater results. If you are interested in the development of 7 × 19 CAR-T, we highly recommend our CAR Design & Construction Service for our clients to build their own 7 × 19 CAR-T cells. we also provide ready to use products such as plasmids vectors, transfected T cells, packaged viral particles and assay kits for 7 × 19 CAR-T cell development.
Reference
Keishi Adachi, Yosuke Kano, Tomohiko Nagai, Namiko Okuyama, Yukimi Sakoda & Koji Tamada.IL-7 and CCL19 expression in CAR-T cells improves immune cell infiltration and CAR-T cell survival in the tumor. Nature Biotechnology doi:10.1038/nbt .4086


