A tool designed to detect the history of viral infection from a drop of blood has been upgraded in the COVID-19 era. VirScan is a technique that determines which of more than 1000 different viruses have infected humans, and can now detect evidence of infection with coronaviruses, including SARS-CoV-2. In a new study, researchers from Bregan Women’s Hospital and Harvard Medical School in the United States provided a number of details about the human antibody response to SARS-CoV-2 and how it might be different in individuals infected with a more severe form of COVID-19.
“In terms of the solution, this is probably the most in-depth serological analysis of any virus,” said Dr. Stephen Elledge, a professor of genetics at Bregan Women’s Hospital. “We now know more and more about the antibodies produced in response to SARS-CoV-2 infection and how often they are produced. The next question is, what is the role of these antibodies? We need to determine which antibodies have inhibitory ability, or which antibodies, if any, may promote the infection of the virus and actually help it enter the immune cells. “
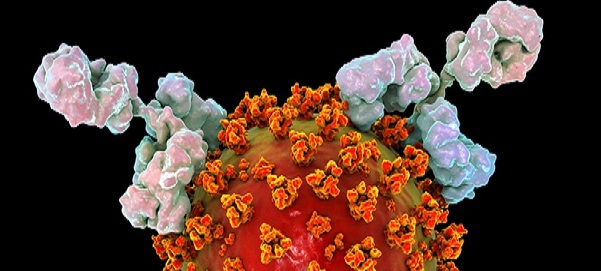
In their analysis, Elledge and colleagues studied the antibody response to SARS CoV-2 by analyzing blood samples from 232 COVID-19 patients and 190 controls before the emergence of COVID-19 using VirScan. They identified eight hundred viral sites called epitopes that could be recognized by the immune system. Not all epitopes are the same, and some epitopes may be recognized by neutralizing antibodies, resulting in a response to the elimination of infection. However, if the body produces antibodies against other epitopes, it may initiate a less effective response, giving the virus an advantage. In some cases, viruses, including the SARS-CoV virus, can even benefit from the body’s antibody response, using antibodies to enter cells, a phenomenon known as antibody-dependent enhancement.
In the case of SARS-CoV-2, the Elledge team detected a range of antibody frequencies specific to different epitopes. Many of the epitopes are public epitope-regions recognized by the immune systems of a large number of patients. One of the common epitopes was identified by 79% of COVID-19 patients. Other epitopes are thought to be private and are recognized only by the immune system of a small number of people or even one person. Ten epitopes exist in the key areas necessary for the virus to enter the host cell and may be recognized by neutralizing antibodies.
The discovery of epitopes by the Elledge team may have an important impact on the vaccine. If it is found that the immune system’s response to public epitopes does not protect or even give SARS-CoV-2 an advantage, then the vaccine needs to target other areas of the virus to power the immune system.
In addition, the Elledge team found that several epitopes are conserved in different coronaviruses, and when infected with SARS-CoV- 2, the immune system is likely to try to reuse antibodies against these epitopes-which is one possible explanation for why many serological tests for COVID-19 produce false positives.
The Elledge team further analyzed where and when different antibody responses occurred and found that patients with severe COVID-19 were more likely to initiate a stronger and broader response to SARS-CoV-2, possibly because their initial immune response failed to control the virus infection early. Among hospitalized patients, men produce more antibodies than women. The authors also compared the history of viral infection in hospitalized and non-hospitalized COVID-19 patients and found that hospitalized patients were more likely to be infected with CMV and HSV-1, two common herpesviruses. However, the authors point out that it is difficult to conclude that there is a causal relationship given that the non-hospitalized patient group is younger and has a higher proportion of whites and women, and that this demographic group usually has a low CMV infection rate.
“Our paper elucidates the antibody response spectrum in patients with COVID-19,” Elledge said. “Next, we need to identify the antibodies that bind to these repeatedly recognized epitopes to determine whether they are neutralizing antibodies or antibodies that may aggravate the patient’s clinical manifestations. This may provide information for the development of improved diagnostic methods and vaccines for SARS-CoV-2. “
