The trend in the field of cancer immunotherapy is the use of cancer vaccines. By using identified tumor antigens to stimulate the immune system, cancer vaccines can generate a specific immune response against tumor cells, thus causing the destruction of these cells and preventing recurrences and metastasis. Recently, a research team led by Zhao Xiao and Nie Guangjun at the National Center for Nanoscience and Technology of the Chinese Academy of Sciences proposed a strategy dubbed “peri-vaccination immune priming,” which involves enhancing the immune system through the use of bacterial nanoparticle vesicles to amplify the subsequent effects of cancer vaccines. The results of the study, titled “Bacteria-derived nanovesicles enhance tumour vaccination by trained immunity”, have been published in the journal Nature Nanotechnology.
A healthy immune system is a prerequisite for the efficacy of cancer vaccines. However, tumor patients often experience distinct immune system dysfunction, in particular severe impairment of antigen-presenting cell function within the innate immune system, which hinders the activation of immune responses by cancer vaccines. The first focus of this study was how to intervene in immune system function during the “peri-vaccination period” to enhance the efficiency of cancer vaccines.
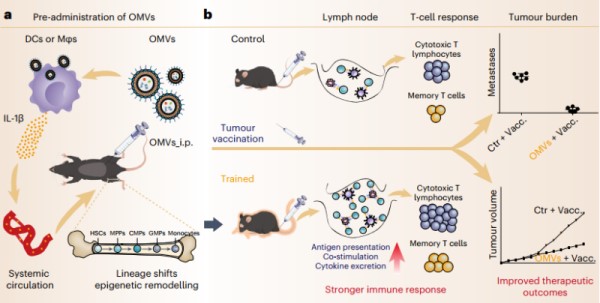
Figure 1. Schematic illustration of immune mobilization based on OMV-induced trained immunity to enhance tumour vaccinations (Liu G, 2023)
With the advancement of research in the field of immunology, scientists’ understanding of the innate immune system continues to deepen. This study used a type of bacterial nanoparticle vesicle known as an outer membrane vesicle (OMV) to stimulate the body to produce a trained immune response before vaccination, thereby enhancing the function of the innate immune system. This strategy, based on nanoparticle vesicles, could fill the clinical application gap in surgical tumor antigen prediction and vaccine preparation.
The team focused their efforts on the research of nano-carriers for cancer vaccines and have developed a variety of nanoparticle carriers based on OMVs, which have effectively improved the immunogenicity of tumor antigens and the immunotherapeutic effects of vaccines. They suggested that research on cancer vaccines should not be limited to optimizing the design of the vaccine itself while ignoring the effect of the body’s immune system function on the efficacy of the vaccine.
Explore some of our tumor antigen targets:
| CD23 | CD9 | CD72 |
| CD28 | CD22 | CD37 |
| CD31 | CD27 | CD33 |
| CD34 | CD36 | CD38 |
| CD48 | CD4 | C5a |
The study also showed that OMVs can stimulate the body to produce a high level of inflammatory factors. These factors, particularly interleukin-1β, can enter the bone marrow, affecting the differentiation process of various progenitor cells during hematopoiesis. The nano-structure of the OMVs played an important role in this process. Under nano-scale, OMVs can deliver pathogen-associated molecular pattern substances, especially lipopolysaccharides (LPS), into the cytoplasm of immune cells, activating the non-classical inflammasome signaling pathway mediated by Caspase11, lead ultimately to the secretion of Interleukin-1β and the induction of trained immunity in the body.
To sum up, the research findings have provided important evidence for the development of safe, highly gene-transfected, and targeted non-cationic mRNA delivery systems to induce durable and robust humoral and cell-mediated immunity for disease treatment.
Reference
Liu G, Ma N, Cheng K, et al. Bacteria-derived nanovesicles enhance tumour vaccination by trained immunity[J]. Nature Nanotechnology, 2023: 1-12.
