Novartis recently announced that its new drug iptacopan has achieved positive results in a Phase 3 clinical trial for the treatment of paroxysmal nocturnal hemoglobinuria (PNH), with patients’ hemoglobin levels increasing significantly after treatment. Novartis expects to submit a regulatory application in 2023, and if approved, it will be the first oral monotherapy in the PNH therapeutic area.
PNH is a rare complement-mediated blood disorder that affects approximately 1-2 people per million people worldwide each year. The complement system is part of the innate immune system that enhances the ability of antibodies and phagocytes to attack and clear pathogens from the body. Patients with PNH have some mutant hematopoietic stem cells, which can cause red blood cells to be destroyed by the complement system, resulting in intravascular and extravascular hemolysis, anemia, thrombosis, fatigue, and a host of other symptoms. Currently, a few anti-C5 therapeutic drugs have been approved for the treatment of PNH worldwide. However, a considerable number of PNH patients still suffer from anemia and fatigue after receiving anti-C5 treatment and require blood transfusions.
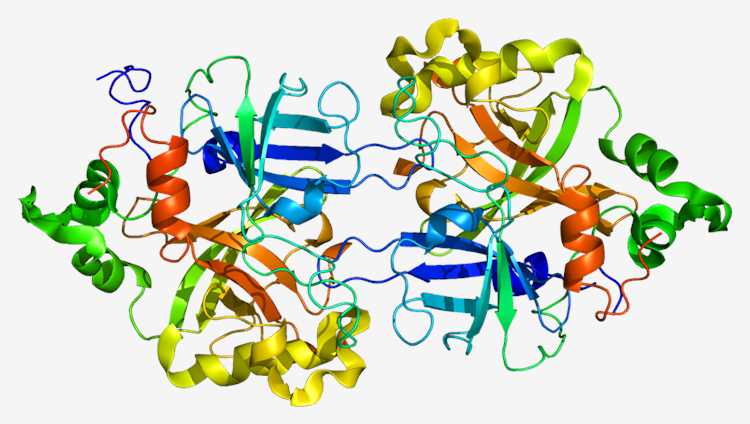
Fig.1 Complement factor B.
Iptacopan is an inhibitory drug that specifically targets complement factor B, a key protein in the alternative complement pathway. Iptacopan prevents both intravascular hemolysis and extravascular hemolysis of PNH by acting upstream of the C5 complement pathway. Iptacopan might be more beneficial for treating patients than anti-C5 therapy, according to the mechanism of action, because it targets the key link in the biological mechanism leading to the occurrence of PNH, providing patients with an oral monotherapy option.
The trial met two primary endpoints, one of which assessed the percentage of patients whose hemoglobin level rose by 2 g/dL or more from baseline after 24 weeks of treatment without blood transfusion, and the other assessed the percentage of participants whose hemoglobin levels remained stable at 12 g/dL or above after 24 weeks without blood transfusion. Secondary endpoints aim to maintain the percentage of participants who remained transfusion-free, mean changes in hemoglobin levels, changes in fatigue, mean changes in absolute reticulocyte count, mean percentage changes in lactate dehydrogenase (LDH) levels, and rates of breakthrough hemolysis and major adverse vascular events.
The top-line results this time showed that patients treated with iptacopan (200 mg twice daily) over 24 weeks increased hemoglobin levels by more than 2 g/dl from baseline compared to patients receiving anti-C5 therapy, and the proportion of people not requiring blood transfusions has increased significantly. In addition, there was a statistically significant increase in the proportion of patients receiving iptacopan treatment who attained a hemoglobin level of 12 g/dL or higher without blood transfusion at 24 weeks compared with anti-C5 therapy, proving that iptacopan was well tolerated and its safety profile was consistent with previously reported data.
It is reported that iptacopan is also being tested in a population of PNH patients who have never received complement inhibitor treatment, and Novartis expects to announce the results in the upcoming months. In addition, Novartis is exploring other indications for iptacopan, including PNH, IgA nephropathy (IgAN), C3 glomerulopathy (C3G), atypical hemolytic uremic syndrome (aHUS), and immune complex-mediated membrane hyperplasia glomerulonephritis (IC-MPGN), all of which have significant unmet medical needs.
Recent progress has been made in PNH treatment, and a wide range of drugs based on different mechanisms of action are actively fighting against their common enemy, hoping to provide patients with diverse curing methods, which has had a significant impact on the development of PNH therapeutics.
Disclaimer: Creative Biolabs focuses on promoting biological and biomedical research globally. This article is for information exchange purposes only. This article is also not a treatment plan recommendation. For guidance on treatment options, please visit a regular hospital.
