CAR-T, Chimeric Antigen Receptor T Cell Immunotherapy, is a new cell therapy that has been developed for many years but has only been improved in recent years. Considered as one of the most promising cancer treatment, CAR-T has a significant effect on the treatment of acute leukemia and non-Hodgkin’s lymphoma. As with all technologies, CAR-T technology has also undergone a long evolutionary process, it is in this series of evolution, CAR-T technology gradually maturing.
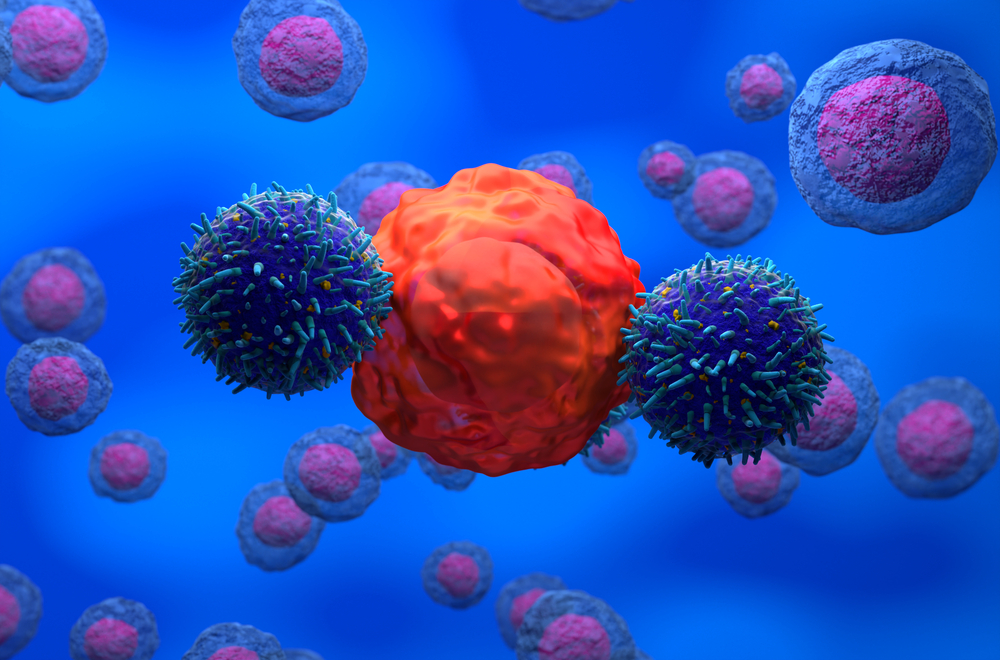
The key to this new therapeutic strategy is the artificial receptors called chimeric antigen receptors (CARs) which recognize target tumor cells, and, after gene modification, the patient’s T cells are able to express this kind of CAR. In human clinical trials, scientists extract some T cells in the patient through a dialysis-like process and then genetically modify them in the lab to introduce the gene that encodes the CAR so that the T cells can express this new receptor. These genetically modified T cells proliferate in the laboratory, and then they are infused back into the patient’s body. These T cells utilize their expressed CAR receptors to bind to molecules on the surface of target cells, and this binding triggers the production of internal signals, which activate these T cells so efficiently that they quickly destroy target cells.
In addition to being used to treat acute leukemia and non-Hodgkin’s lymphoma, CAR-T immunotherapy has also been used in recent years to treat diseases such as solid tumors, autoimmune diseases, HIV infection and transplant rejection. Here we summarize some of the latest progress in CAR-T research area for our client, and hope this information may be of help to your research work.
1. Nat Med: New CAR-T cell therapy is expected to treat B-ALL leukemia
In a new study, researchers took patients with B-cell acute lymphoblastic leukemia (B-ALL) as experimental subjects in Phase I clinical trial to test a novel cell therapy based on CAR-T technology.
And they have successfully treated B-ALL that is resistant to a previous CAR-T cell immunotherapy. Relevant findings were published online in the journal Nature Medicine on November 20, 2017, titled “CD22-targeted CAR T cells induce remission in B-ALL that is naive or resistant to CD19-targeted CAR immunotherapy.“
This cellular therapy involves extracting millions of T cells from a patient, genetically modifying them so that they can destroy malignant cancer cells and subsequently perfusing them back into the patient. This genetic modification introduces a chimeric antigen receptor on the surface of T cells that targets a specific protein molecule found on the surface of cancer cells from leukemia and lymphomas. Now researchers from Medicine School in Stanford University and the U. S. National Cancer Institute (NCI) devised a new CAR-T-cell therapy that targets a surface molecule called CD22.
This Phase I trial recruited 21 children and young adults (aged 7 to 30 years) with B-ALL who had either had a relapse or did not respond to previous therapies. 15 of these patients have also received CAR-T cell therapy targeting CD19, but no significant improvement has been achieved. These patients were given different doses of this new CD22-targeted CAR-T cell therapy. Of the 6 patients who received the lowest dose of treatment, 1 achieved a complete remission after treatment. Among those who received higher doses, 73% achieved relief. Although a minority of patients remain completely relieved after up to 21 months of treatment, most patients have a relapse.
2. Allogeneic CAR-T Therapy UCART123 Expands AML and BPDCN Treatment Indications Clinical Study Supported by FDA
On November 6, Cellectis, a company dedicated to allogeneic CAR-T development, announced that the FDA permitted the clinical trial UCART123, a CAR-T therapy, to continue and extends the treatment of acute myeloid leukemia (AML) and blast cells Clinical trials of plasmacytoid dendritic cell tumor (BPDCN).
UCART123 is a versatile CAR-T therapy that is different from traditional autologous CAR-T therapy. In traditional CAR-T therapies, researchers first need to extract T cells from patients and insert chimeric antigen receptors (CARs) to target T cells to specific antigens on cancer cells. At last, these engineered T cells are reintroduced to the patient’s body to treat cancer. The universal CAR-T therapy can prepare all-T cells in advance with the advantages of treatment at any time. UCART123 can specifically target CD123 antigens that are commonly expressed on AML as well as on the surface of BPDCN cancer cells. The treatment was launched in February this year as the first FDA-approved universal CAR-T treatment to enter clinical trials.
Like traditional CAR-T therapy, UCART123 also poses a safety risk. One patient died in a clinical trial, and the FDA suspended the trial on September 4, requiring Cellectis to redesign safely. Following discussions with the FDA, Cellectis decided to make the following changes to the current clinical phase 1 trial of UCART123:
- Reducing the number of UCART123 cells to 62500 cells per kilogram
- Reducing the amount of cyclophosphamide administered daily to every square foot 750 mg of rice for 3 days. The maximum daily dose will not exceed 1.33 grams
- Introducing specific criteria on the day of UCART 123 cell infusion, including the absence of a new uncontrolled infection following lymphocyte clearance, no fever and organ dysfunction, and only replacement doses of glucocorticoid.
- Ensuring that the next 3 patients in each treatment are younger than 65 years of age
- Ensuring that the next patient recruitment is staggered in both AML123 and ABC123 scenarios and patient recruitment interval should not be less than 28 days.
3.Cancer Discov: The new discovery is expected to reduce the side effects of CAR-T therapy
While cancer researchers are excited by the FDA approval of the recent Novartis CAR-T therapy Kymriah, concerns about its side effects remain troubling to the academic community. In Novartis’s trials of similar therapies, some patients developed a dangerous immune response called cytokine release syndrome and some had neurotoxicity. Serious side effects can be life-threatening. Recently, researchers at Fred Hutch, a Fred Hutchinson cancer research center, said they found biomarkers associated with cytokine release syndrome and neurotoxicity and they have built algorithms to predict how dangerous these side effects are. Their research is published in a recent issue of Cancer Discovery.
In order to find biomarkers of side effects, the researchers followed closely 133 patients who participated in the CAR-T trial developed by the center for the treatment of chronic lymphocytic leukemia, non-Hodgkin’s lymphoma or acute lymphoblastic leukemia. They documented the timing and course of symptoms and detailed pathology and imaging. Most patients developed cytokine release syndrome. The majority found themselves in remission spontaneously, but 10 patients had serious symptoms.
One of the hallmarks of patients with severe cytokine release or neurotoxicity is that endothelial cells in the inner walls of their blood vessels become over-activated, drawing the conclusion that the detection of endothelium-activated biomarkers can help identify CAR-T-treated patients at highest risk of serious side effects.
The researchers pinpointed two key criteria for predicting severe cytokine release syndrome, including a fever of at least 38.9 degrees Celsius (102 degrees Fahrenheit) and a high level of immune-related cytokine MCP-1. Researchers said that patients with high levels of IL-6 also have an increased risk of neurotoxicity. Most neurotoxic conditions are preceded by cytokine release syndrome, although more studies are needed to determine the link between the two.
(doi: 10.1158/2159-8290.CD-17-0698)
4.CAR-T therapy caused death, clinical research was suspended by the FDA for patient death
On Sept. 4, Cellectis, a French biotechnology company focused on the development of allogeneic CAR-T cell therapy (UCART), received a notification from the FDA, requiring the suspension of clinical phase 1 trials of cell-based therapies UCART123, which respectively belonged to the treatment of acute myeloid leukemia (AML) and somatic cell-like dendritic cell tumor (BPDCN).
The clinical trial suspension resulted from one patient death in a clinical trial of Cellectis for the treatment of BPDCN (ABC study). It is the first 78-year-old male patient in the BPDCN study who had previously received one treatment. The patient suffered from recurrent / refractory BPDCN with 30% of blast cells in the bone marrow and biopsy confirmed skin lesions. The pretreatment regimen that he received was fludarabine at 30 mg / m2 / day for 4 days and cyclophosphamide at 1 g / m2 / day for 3 days. On Day 16, 2017, the patient received 6.25 x 105 UCART123 cells per kilogram of Kg, the first dose set by the protocol with no complications. On day 5, the patient developed cytokine release syndrome (CRS) in 2nd level and lung infection in 3rd level, both of which are improved after receiving initial drug and anti-infective therapy of tocilizumab. On day 8, the patient presented with CRS in 5 level together with leprosy leak syndrome in 4 level.
Despite the treatment of corticosteroids, 2-fold tociluzumab and intensive care, the patient still died on the 9th day.
Cellectis is currently working closely with clinical researchers and the FDA to resume the trial’s resumption by modifying the protocol, including reducing the dose of UCART123.
5. Nat Commun: Nanotechnology and Precision Medicine Provide New Aid for Tumor Immunotherapy
A new biomedical tool that uses nanoparticles to deliver genes to target cells facilitates the resolution of many diseases, including cancer, diabetes and HIV, which is faster, cheaper and easier than traditional therapies. This tool was developed by researchers from Fred Hutchinson Cancer Center. Related pre-clinical trial results were published in the latest issue of Nature Communications.
Developed by Matthias Stephan et al., this nanoparticle-based drug delivery system expands the therapeutic potential of mRNAs by delivering RNA directly into body cells and thereby directing the body to encode proteins that resist disease. Genetic regulation through the transport of mRNA can play a short-term change in gene expression characteristics, which will not change the original genetic information in the cell, so as to avoid the inevitable impact on the body.
Stephan et al. used three examples to demonstrate the reliability of their technology:
- Native T cell receptors were engineered using nanoparticles to carry T-cell gene editing tools, which were then ligated with the gene encoding “chimeric antigen receptor CAR) “genes, so that the modified T cells can target tumor cells to attack.
- The nanoparticles carry mRNA that can promote the replication of hematopoietic stem cells, thereby accelerating the rate of hematopoietic stem cell proliferation, and replacing the original cancer cells in the body through bone marrow transplantation way
- Nanoparticles carry mRNA and foxo1 mRNA that can transform CAR-T cells to equip anti-cancer T cells with the memory ability and eventually form long-term anti-cancer properties.
(doi:10.1038/s41467-017-00505-8)