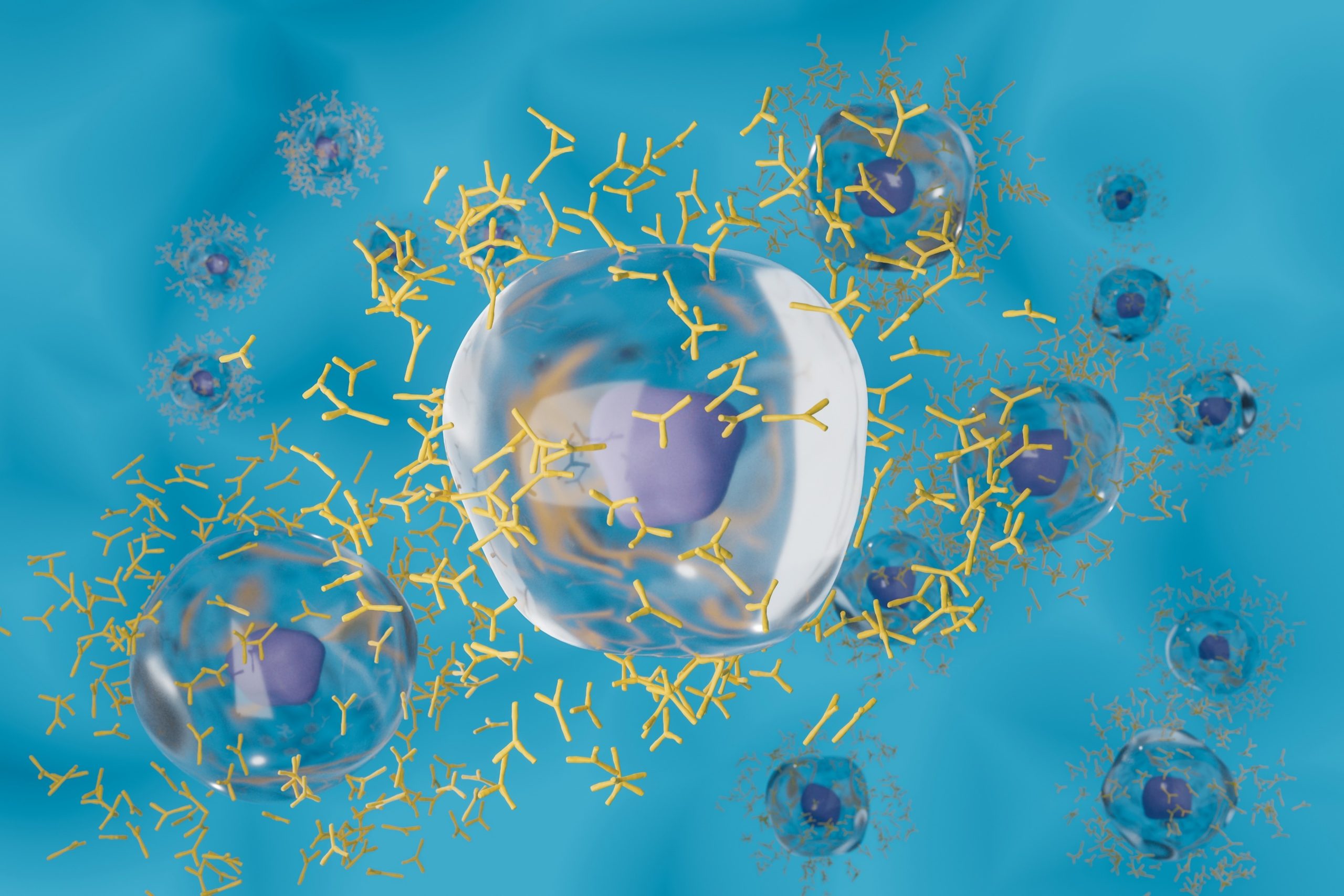
Antibodies are a class of proteins that are important to the body’s immune system. Immunoglobulin G (IgG) stores memories of past infections and marks dangerous microbes so they can be destroyed by immune cells. Researchers have known for decades that the body’s white blood cells, plasma B cells, produce IgG. Plasma B cells are so efficient that they can produce more than 10,000 IgG molecules per second. However, researchers are currently unclear about the molecular mechanism behind what causes plasma cells to secrete antibodies into the blood.
To further understand these mechanisms, the researchers conducted an unprecedented analysis. They captured thousands of single plasma B cells and their secretions, then correlated the amount of protein released by each cell with a map of the tens of thousands of genes expressed by that cell. To collect cells and their secretions, researchers use tiny, bowl-shaped hydrogel containers (nanovials). The analysis showed that genes involved in producing energy and eliminating abnormal proteins were more important for the secretion of large amounts of IgG than genes containing the instructions for making the antibodies themselves. Additionally, they found that the presence of the CD59 gene, a gene not previously associated with IgG secretion, was a better predictor of mass-producing plasma cells than other genetic markers associated with these cell types.
Researcher Dino Di Carlo said that these processes in the cell are like an assembly line for making proteins, with bottlenecks appearing in many places, and everything in the cell must proceed smoothly and simultaneously. If a cell is making a lot of protein, it’s using up a lot of energy, so we need a way to correct the messed-up proteins. These findings not only promote researchers’ basic understanding of biology but also have certain clinical significance in the field of biomedical research. For example, by knowing which genes are involved in producing large amounts of antibodies, drugmakers can engineer cells to secrete large amounts of them. This information also holds promise for an emerging strategy to introduce engineered cells directly into patients.
The new approach, using nanovials and standard laboratory equipment, also opens up the possibility of understanding how DNA instructions are translated into cellular behavior. Each nanovial contains special molecules that custom-bind to proteins on the surface of the cell the researchers are investigating, allowing the nanovial to capture one cell at a time. Once the cells are immobilized and protected in the nanobowls, their secretions accumulate and adsorb to specific antibodies designed to capture them. In this study, the researchers placed tens of thousands of plasma cells and the IgG they released into nanovials, and then used instruments to analyze the mRNA of each cell in the nanovials. Every cell in the human body carries the same blueprint written in DNA. Therefore, researchers can detect which genes are active by looking at the mRNA, which translates the instructions so that each cell can make the protein that matches its function. Researcher Carlo said, “Every cell has multiple layers of information, and we can connect the last layer (the actual amount of secreted protein with a clear function in the human body) to the most basic layer of genetic code.” Now that researchers have the methods, the most interesting question for them is what questions to ask next. In future studies, the researchers hope to identify information on all genes that influence the production and secretion of IgG by plasma cells. Therefore, the researchers developed a new method to link secretion quantity with single-cell sequencing (SEC-seq), allowing researchers to explore more deeply the association between genome and function and laying a certain foundation for discoveries in immunology, stem cell biology, and other research fields.