PIn a new study, Spanish researchers have developed a cell therapy for a type of leukemia for which there are currently few treatment options. This STAb-T cell therapy is based on STAb-T cells and has shown potential to treat patients with T-cell acute lymphoblastic leukemia (T-ALL) who have failed to respond to chemotherapy or bone marrow transplantation. The results of the study were recently published in Journal for ImmunoTherapy of Cancer under the title “Efficient preclinical treatment of cortical T cell acute lymphoblastic leukemia with T lymphocytes secreting anti-CD1a T cell engagers”.
PT-ALL is a rapidly progressive type of leukemia caused by the abnormal proliferation of T cells called lymphoblasts (immature white blood cells) in the bone marrow and blood. It is a so-called rare disease that accounts for approximately 10% to 15% of all acute leukemias diagnosed in children and 20% to 25% of acute leukemias affecting adults. In total, around 100 cases of T-ALL are detected each year only in Spain.
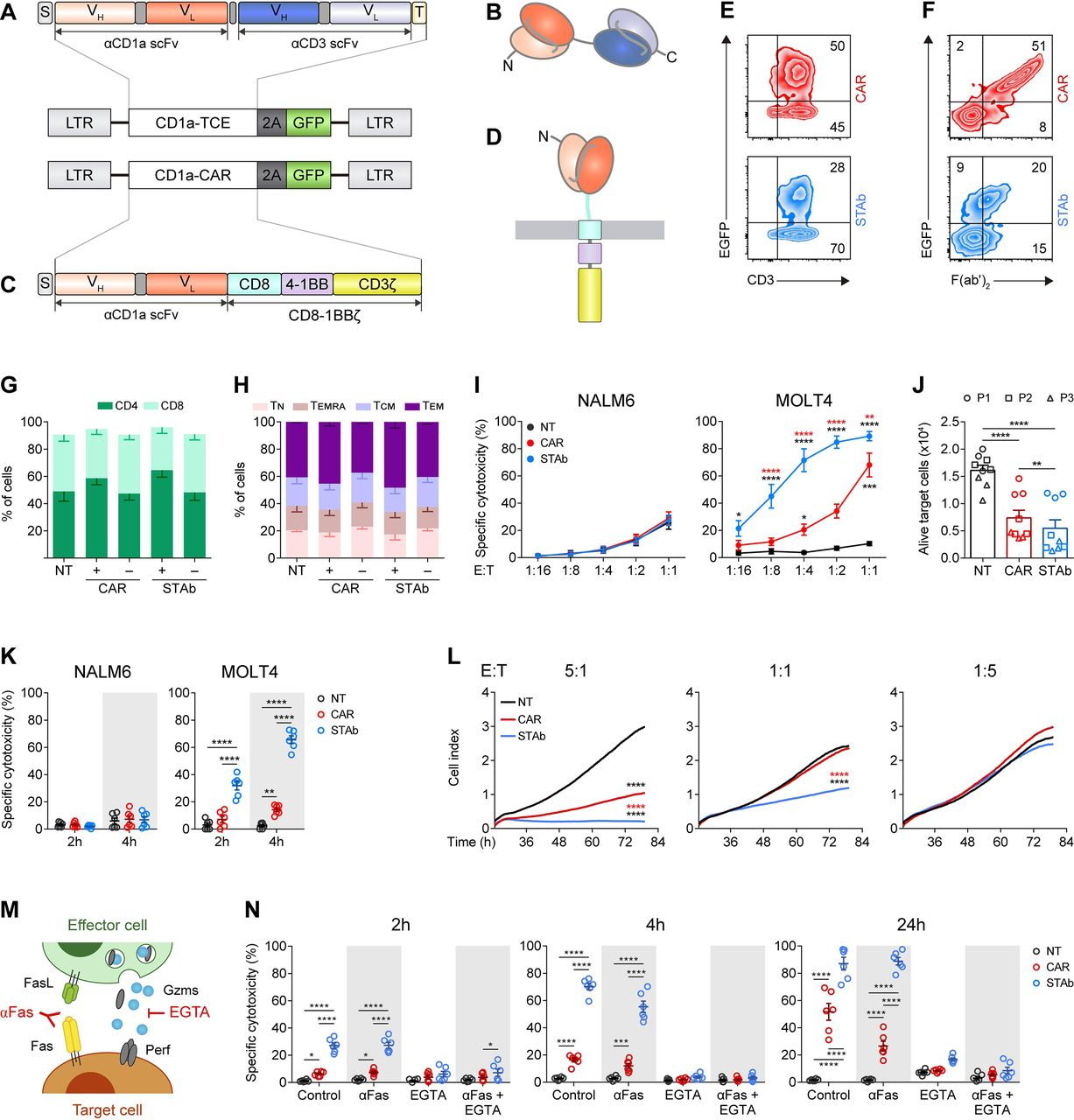
PSTAb-T cell therapy is an evolution of CAR-T cell therapy. In contrast to CAR-T cell therapy, in which T cells express a receptor with a monospecific antibody that recognizes only one target on the surface of the tumor, STAb-T cell therapy has the advantage that it is based on the secretion of a specific type of bispecific antibody that recognizes two targets: one located on the tumor cells and the other on the T cells. In this way, the bispecific antibody forms an artificial bridge that allows the therapeutic T cells to come into contact with the tumor cells, promoting their elimination and keeping the healthy T cells safe.
PFor the treatment of T-ALL, this distinction is crucial. In the case of B-cell acute lymphoblastic leukemia (B-ALL), CAR-T cells recognize a target and destroy both diseased B cells and healthy B cells. Patients receiving this therapy can live a normal life, but this thanks to the regular supply of antibodies obtained from healthy donors.
PIn T-ALL, the application of CAR-T cell therapy is even more difficult because the immune cells used to fight the tumor, the T cells, are identical to the diseased cells, and their use leads to a state of immunodeficiency. Furthermore, no alternative therapies are available, as is the case with B-ALL.
PSTAb-T cell therapy may be an improvement on CAR-T cell therapy, especially in relapsed patients with reduced numbers of normal T cells. These authors found STAb-T cells to be very effective in both in vitro and in vivo animal models. Different options are being considered to bring this therapy into clinical trials.
PImmunotherapeutic strategies and adaptive cell therapy are still only benefiting a small number of patients. Dr. Luis Álvarez-Vallina, the co-corresponding author of the paper, explains that it is necessary to develop strategies for very specific targets for each disease and to adapt them for each patient. According to him, the future of cancer and leukemia research lies in the development of personalized therapies that offer options to all those who are currently not suitable for conventional therapies. STAb-T therapies are on this path.
PDr. Alvarez-Vallina concludes that STAb-T cell therapy is a completely new therapy that represents an innovation in the field of cell therapy, and can be applied to a wide range of cancer types, some of which are in clinical development.
Reference
1. Jiménez-Reinoso, Anaïs, et al. “Efficient preclinical treatment of cortical T cell acute lymphoblastic leukemia with T lymphocytes secreting anti-CD1a T cell engagers.” Journal for Immunotherapy of Cancer 10.12 (2022).