Flaviviruses, which belong to the family Flaviviridae, are encoded by a single-stranded, positive sense RNA genome approximately 11 kb in length. The genome is a single open reading frame encoding 10 viral proteins that are cleaved co- and post-translationally from the polyprotein, the capsid (C), membrane (M), and envelope (E) structural proteins and the nonstructural (NS) proteins 1, 2A, 2B, 3, 4A, 4B, and 5. As of 2013, the International Committee on Taxonomy of Viruses has classified 53 different viral species as belonging to the genus Flavivirus. However many newly identified flaviviruses are being isolated each year and remain to be formally described. Of these 53 separate species, 40 have been associated with infection in humans such as Dengue virus (DENV), yellow fever virus (YFV), tick-borne encephalitis virus (TBEV), Japanese encephalitis virus (JEV), and West Nile virus (WNV). Several flavivirus species including JEV, WNV, and louping ill virus also cause diseases of economically important livestock and poultry. In light of the heavy disease burden attributed to flaviviruses, the generation of effective vaccines and therapeutics remains a significant goal within the medical research community.
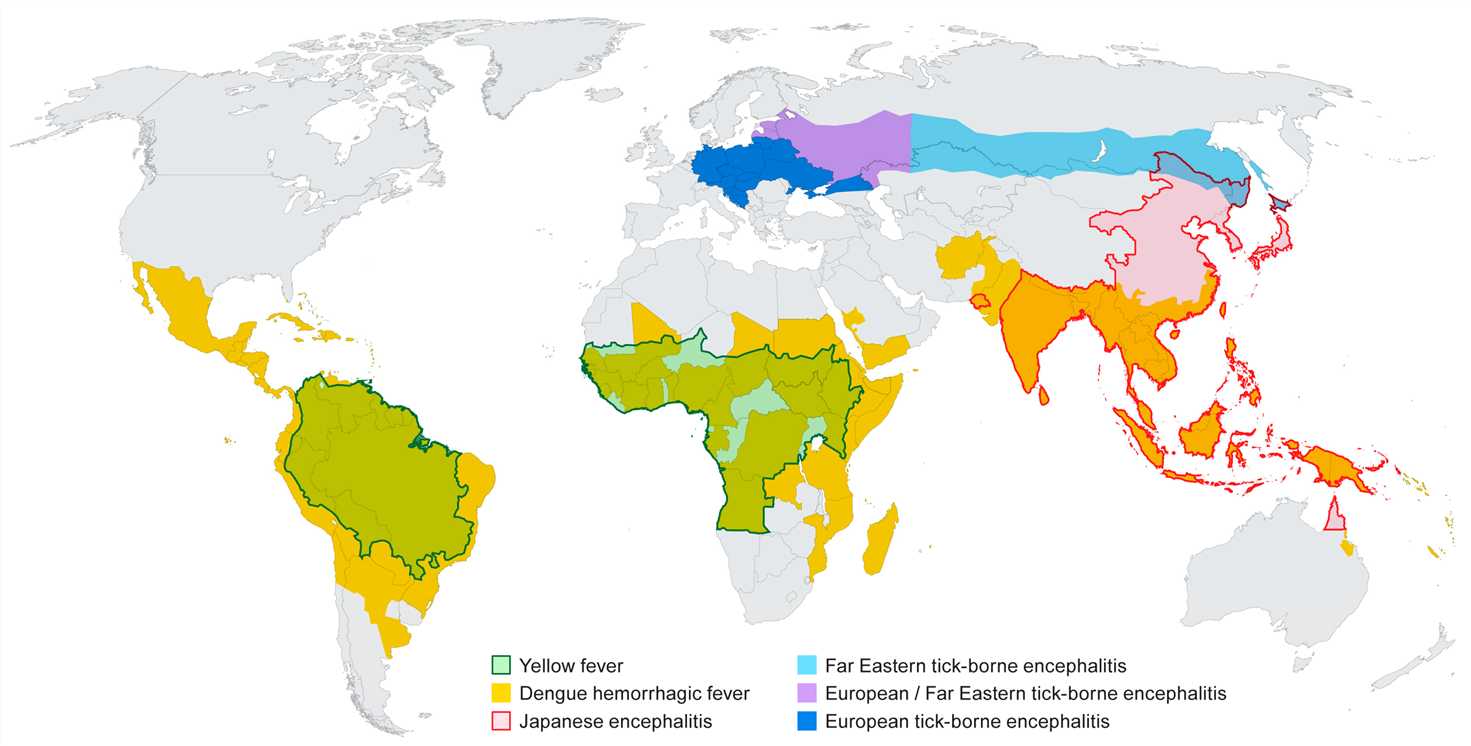
Since the first isolation of DENV in 1943, four types have been identified. Dengue viruses are often considered the most important arboviruses worldwide causing an estimated 50–100 million infections per year and posing a threat to 2.5 billion people in tropical and subtropical regions. Although the majority of infections lead to self-limited febrile illness, the severe form of the disease can lead to life-threatening dengue hemorrhagic fever which has a mortality rate of 2.5%. The usual urban transmission route of all four serotypes of DENV is generally mediated by Ae. albopictus and Ae. aegypfi mosquitoes.
The spectrum of illness seen with dengue includes a mild nonspecific febrile syndrome (often in younger children), classic dengue, dengue hemorrhagic fever (DHF), and dengue septic shock (DSS). Also known as “Seven Day Fever”, the course of dengue disease can be divided into three phases: febrile phase, critical phase and convalescent (or reabsorption) phase.
Since the signs of dengue fever can be easily confused with malaria, leptospirosis and typhoid fever, the diagnosis of this disease is difficult. Some laboratory tests can be used in the detection of dengue viruses, but the results usually come back too late to help direct treatment decisions. Sanofi Pasteur released the first licensed dengue vaccine, Dengvaxia, in December 2015. It is currently licensed for use in the Phillipines, Mexico, and Brazil in people between 9 and 45 years of age. In clinical trials, the vaccine efficacy for the four dengue serotypes is different and other vaccine candidates are currently under clinical trials. The disease can be prevented by avoiding mosquito bites. The Aedes mosquitoes responsible for transmission bite during the day. Bites are best avoided by wearing DEET mosquito repellent or permethrin-impregnated clothing when outdoors. Aedes mosquitoes also bite indoors, so having screened windows or air-conditioning can reduce mosquito abundance indoors.
YFV, most of which is arthropod-borne, is acquired from mosquito bites in tropical regions worldwide. Yellow fever is differentiated from malaria by the presence of conjunctival suffusion or relative bradycardia and by its short incubation period.
Disease caused by YFV may be subclinical, mild and non-specific, or severe with jaundice, hemorrhage, and death. The first phase of disease, which starts 3–6 days after the bite of an infective mosquito, is non-specific and may include fever, malaise, dizziness, nausea and vomiting, headache, lumbosacral pain, and myalgia. The remission phase either proceeds recovery or may be followed by a period of intoxication characterized by headache, vomiting, jaundice, enlargement of the liver and hemorrhage. More than 90% of cases occur in sub-Saharan Africa.
A presumptive diagnosis can be made based on the patient's clinical features, dates and places of travel, activities, and epidemiologic history of the location where the presumed infection occurred. Laboratory diagnosis is usually performed by testing of serum to detect virus-specific IgM and neutralizing antibodies. Sometimes the virus can be found in blood samples taken early in the illness. In fatal cases, polymerase chain reaction (PCR), histopathology with immunohistochemistry, and virus culture of biopsy or autopsy tissues can also be effective. There is no medicine to treat or cure infection from yellow fever. Rest, drink fluids and pain relievers and medication can be used to reduce fever and relieve aching. Avoid certain medications, such as aspirin or other nonsteroidal anti-inflammatory drugs, for example ibuprofen (Advil, Motrin), or naproxen (Aleve), which may increase the risk of bleeding. The most effective way for prevention is to prevent mosquito bites.
Japanese encephalitis (JE) is an inflammatory disease of the brain caused by JEV. JE is the most common cause of viral encephalitis in Asia, from the China-Russia border region in the north to the northern Australia in the south, and from the Western Pacific islands in the east to the India-Pakistan border region in the west. There are approximately three billion humans are at risk of contracting JEV via the bite of Culex mosquitoes, especially Cx. tritaeniorhynchus and Cx. vishnui which are associated with rice farming in Asia. According to World Health Organization data, there are 30,000-50,000 clinical cases reported annually with a 5%–30% case fatality rate. Approximately 30%–50% of surviving patients experience permanent neuropsychiatric sequelae which creates significant challenges to long-term healthcare and results in severe economic loss.
The incubation period is typically 5-15 days before developing symptoms. Initial symptoms often include fever, headache, and vomiting. Mental status changes, neurologic symptoms, weakness, and movement disorders might occur in few days. Seizures are common, especially among children.
JEV produces a high inapparent to apparent infection ratio, ranging from 25:1 to 500:1 case of encephalitis. However, when encephalitis occurs, the mortality rate is in the range of 20 to 50%. Some patients will only show an undifferentiated febrile illness or have mild respiratory tract complaints. The diagnosis is usually made serologically as virus isolation is not usually successful. No specific treatment is available. An inactivated suckling mouse brain vaccine has been available since the early 1960s which has been extensively used throughout Asia. The efficacy rate ranges from 60 to 90%. The most effective way to prevent infection from JEV is to prevent mosquito bites.
WNV is a neurotropic flavivirus that is endemic in many parts of the world. Originally isolated from a febrile patient in Uganda in 1937, WNV was introduced into North America in 1999, and is now the leading cause of mosquito-borne and epidemic encephalitis in the United States. Typically, arboviruses infect a limited number of vectors with transmission cycles often involving just two or three key species.
Most people infected with WNV may have fever and some pains.
No vaccine or specific antiviral treatments for WNV infection are available. In order to reduce fever and relieve some symptoms, over-the-counter pain relievers can be used. Patients may need to be hospitalized to receive supportive treatment, such as intravenous fluids, pain medication, and nursing care. The most effective way to prevent infection from WNV is to avoid mosquito bites. Use insect repellent, wear long-sleeved shirts and pants, treat clothing and gear, and take steps to control mosquitoes indoors and outdoors.
References: