Metabolism is the chemical process your body uses to turn the food you eat into life-sustaining fuel. Food includes proteins, carbohydrates and fats. These substances are broken down by enzymes in the digestive system, which are then taken to cells as fuel. Your body either uses them immediately or stores them in liver, fat and muscle tissue for later use.
Metabolic diseases occur when the metabolic process fails, resulting in too much or too little of the essential substances needed by the body to maintain health. Our bodies are very sensitive to metabolic errors. The human body must have amino acids and a variety of proteins to perform all its functions. For example, the brain needs calcium, potassium and sodium to produce electrical impulses, while lipids (fat and oil) need to maintain a healthy nervous system. There are many forms of known metabolic disorders. These include:
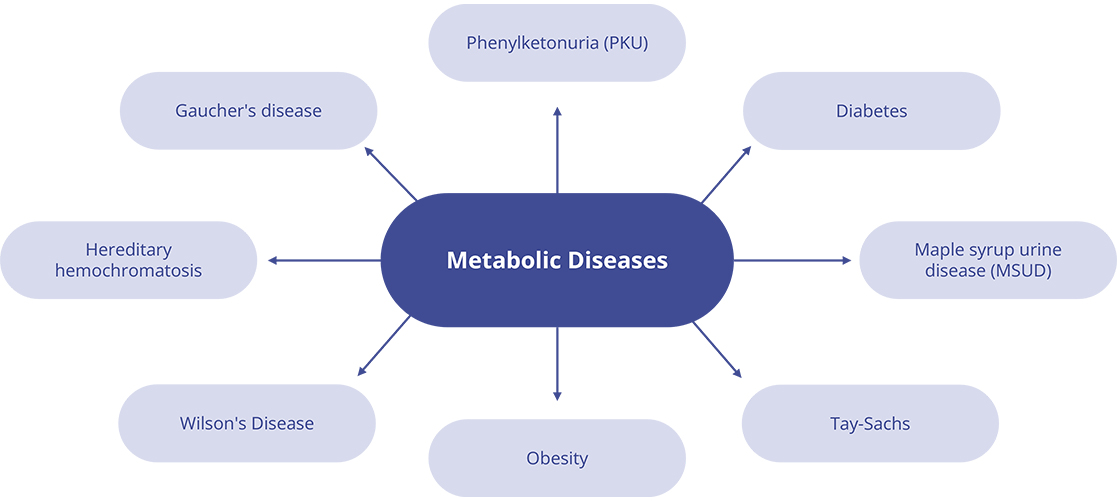 Fig.1 Types of metabolic diseases.
Fig.1 Types of metabolic diseases.
Metabolic diseases can occur at birth, many of which can be identified by routine screening. If the metabolic disorder is not detected early, it may be diagnosed in later life when symptoms appear. Special blood and DNA tests can be used to diagnose genetic metabolic disorders. In addition, in terms of pathophysiological/mechanistic interactions, abnormal gut microbiota also can play a role in the diagnosis of metabolic disorders.
In recent decades, the incidence and prevalence of metabolic disorders such as insulin resistance, type 2 diabetes, dyslipidemia, and metabolic syndrome have risen sharply. Although there are several drugs to choose from, due to the inherent genetic variability of the population and the lack of specific clinical trials, only a small percentage of patients are effective for the treatment. Human induced pluripotent stem cells (hiPSCs) and the recent genome-wide association studies (GWAS) have made high-throughput pharmacological screening analysis possible, which will enable the development of effective treatment methods based on precision medicine.
Recent studies have linked changes in energy metabolism to the fate of iPSCs. In the 10 years since the first discovery of epigenetic reprogramming into iPSC, many different groups have been modeling various genetic diseases, in part because of its ease, accessibility, and commercialization.
Obesity is a risk factor for the development of insulin resistance, diabetes, metabolic syndrome, cancer and osteoarthritis, and therefore reduces the quality of life and life expectancy. Endothelial cells (ECs) derived from human embryonic stem cells (hESCs) have been evaluated in models of myocardial infarction and hind limb ischemia, and used for angiogenesis and neovascularization treatments. Several research groups have evaluated the derived form of hiPSC-EC, and the results showed that hiPSC-EC derived from diet-induced obesity (DIO) mice exhibited reduced vascular function in vitro, reduced function in vivo, and vascular incorporation into the host. This may lead to discoveries of hiPSC-EC therapy for patients in pre-diabetic people or obese patients with peripheral vascular disease.
T2DM is a disease characterized by genetic, epigenetic, environmental or lifestyle risk factors that cause abnormal insulin secretion by pancreatic β cells. iPSCs were derived from the epidermal keratinocytes of elderly T2DM patients, and it was observed that this iPSC can restore the rejuvenated state, which shows telomere lengthening and inhibits senescence-related p15INK4b/p16INK4a gene expression and oxidative stress signaling, leading to regenerative medicine applications.
Metabolic diseases usually destroy the normal cellular processes of the heart and cause cardiac dysfunction, life-threatening arrhythmias, and ultimately increase mortality. Due to the morbidity associated with tissue biopsy and the lack of tissue availability, modeling of in vitro metabolic diseases using human heart tissue presents challenges. In recent years, researchers have used patient-specific iPSC-derived cardiomyocytes (iPSC-CM) to study various cardiomyopathy and heart channel diseases, including arrhythmogenic right ventricular cardiomyopathy, familial dilated cardiomyopathy, familial hypertrophy Cardiomyopathy and long QT syndrome. The use of the iPSC-CM platform to replicate the research progress of obvious mutation-induced cell disorders has also made it possible to study harmful metabolic diseases in Petri dishes.
For Research Use Only. Not For Clinical Use.