Liver Organoids Introduction
The liver, a vital organ with a remarkable capacity for regeneration, plays a central role in metabolism, detoxification, and immune function. However, its complex architecture and diverse cellular composition make it challenging to study in a traditional cell culture setting. Animal models, while valuable, often fail to fully recapitulate human liver physiology and disease mechanisms. In recent years, a groundbreaking technology known as organoids has emerged, offering a powerful new platform for biological research. Liver organoids are miniature, three-dimensional (3D) cell grown in a lab that closely mimic the architecture and function of the human liver. Liver organoids are used in various fields such as drug discovery and drug toxicity assessment.
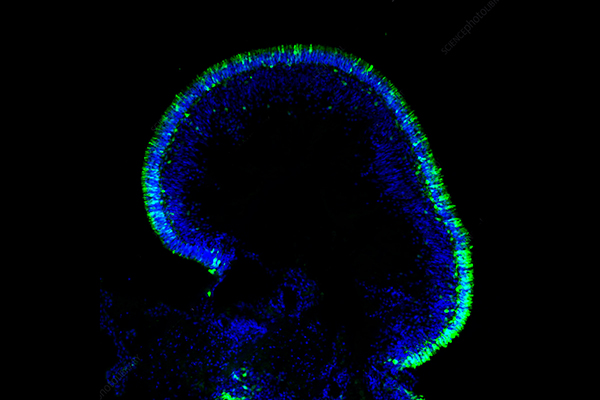
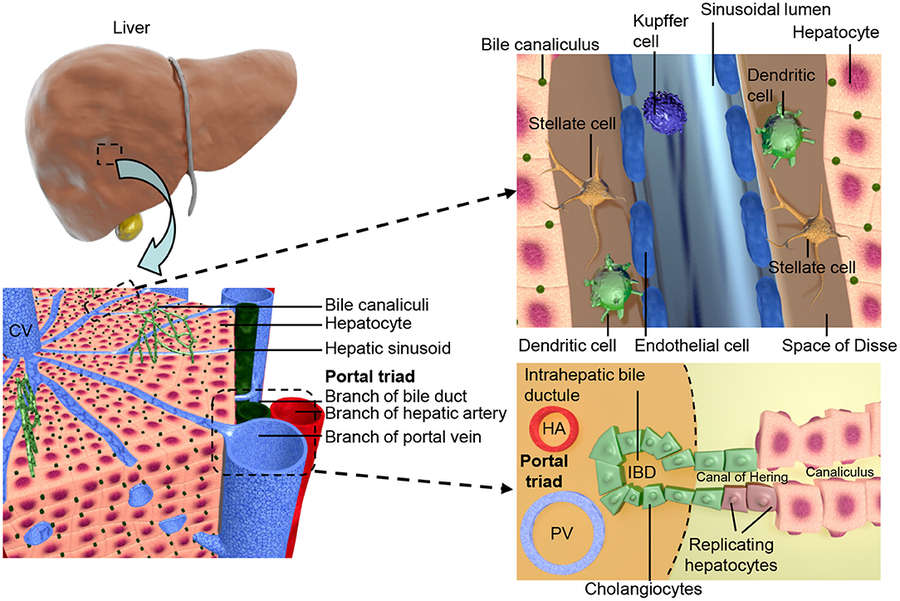 Figure 1 Shows the structural organization of the liver at different scales.1,5
Figure 1 Shows the structural organization of the liver at different scales.1,5
What Are Liver Organoids?
Liver organoids are self-assembling, 3D multicellular structures derived from pluripotent stem cells (PSCs) or adult liver stem/progenitor cells that mimic key aspects of the native human liver's architecture and function. Unlike conventional 2D cell cultures, organoids spontaneously organize into complex structures that resemble the in vivo tissue, exhibiting cellular differentiation, intercellular interactions, and tissue-specific functions. They typically contain various liver cell types, including hepatocytes (the main functional cells of the liver), cholangiocytes (cells lining the bile ducts), and sometimes even stellate cells and endothelial cells, replicating the liver's intricate cellular diversity.
Categories of Liver Organoids
Liver organoids are self-organizing 3D structures composed of multiple liver-specific cell types, including hepatocytes, cholangiocytes (bile duct cells), and occasionally endothelial or stromal cells. They are categorized into two main types:
Simple organoids
-
Hepatocyte organoids: Derived from primary hepatocytes or iPSCs, forming clusters with metabolic functions.
-
Cholangiocyte organoids: Generated from bile duct cells, forming cystic structures.
Complex organoids
-
Hepato-biliary organoids: Combine hepatocytes and cholangiocytes, often using iPSCs or adult liver progenitor cells.
-
Vascularized organoids: Incorporate endothelial cells to simulate blood vessel networks, enhancing physiological relevance.
Generation Methods of Liver Organoids
The two main methods for the generation of liver organoids are:
 Liver tissue-derived organoids
Liver tissue-derived organoids
These are generated from adult bile duct-derived bipotent progenitor cells, fetal hepatocytes, or surgically resected tumor tissues. The process involves isolating single liver cells and culturing them in a specific medium.
 Pluripotent stem cell-derived liver organoids
Pluripotent stem cell-derived liver organoids
These are developed from ESCs or iPSCs. Their generation involves a multi-step differentiation process, including endodermal differentiation, hepatic specification, and final hepatic maturation leading to liver organoid formation.
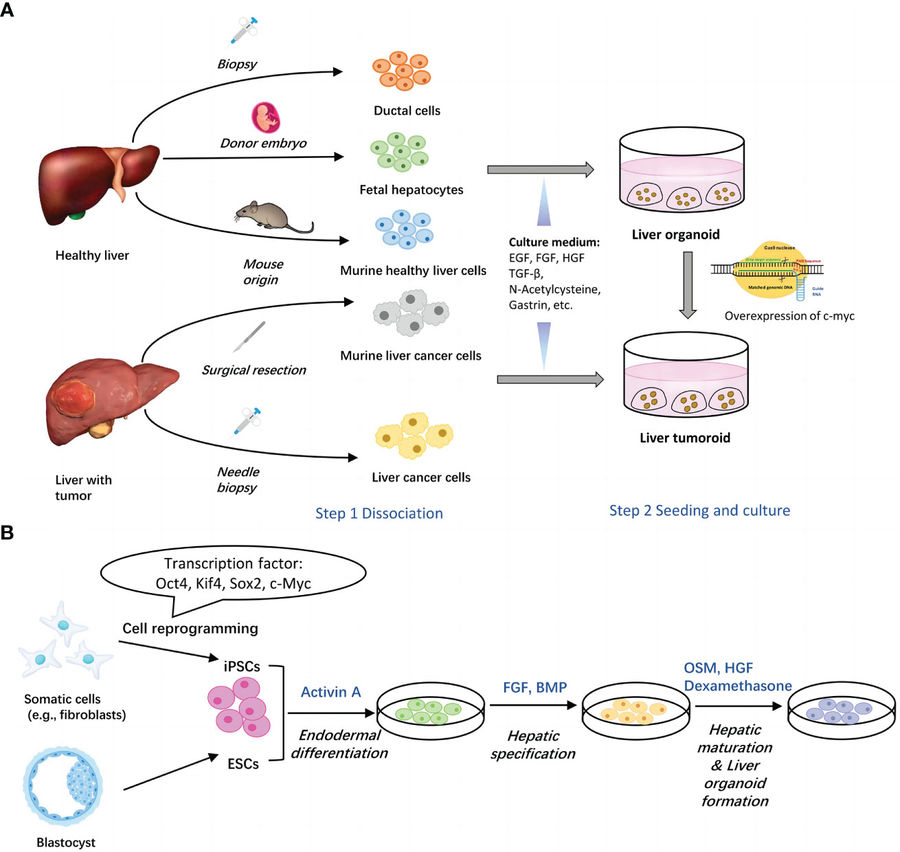 Figure 2 Two main methods for generation of liver organoids.2,5
Figure 2 Two main methods for generation of liver organoids.2,5
Applications of Liver Organoids
Disease Modeling
Liver organoids provide invaluable in vitro models for studying various liver diseases, including non-alcoholic fatty liver disease (NAFLD), non-alcoholic steatohepatitis (NASH), viral hepatitis (e.g., HBV, HCV), genetic liver disorders (e.g., α1-antitrypsin deficiency), and liver cancer. Researchers can introduce disease-causing mutations, expose organoids to toxins, or infect them with viruses to recapitulate disease phenotypes and investigate underlying molecular mechanisms.
Table 1. Organoid-based models of liver disease.3,5
|
Disease
|
Species
|
Organoid source and derivation
|
|
Alagille syndrome
|
Human Mouse
|
Adult tissue (surgical resection), iPSCs (fibroblast-derived), Adult tissue (GEMM)
|
|
Alcohol-related liver disease
|
Human
|
ESCs
|
|
Alpha-1 antitrypsin deficiency
|
Human
|
Adult tissue (surgical resection; liver transplantation; biopsy)
|
|
Citrullinemia type I
|
Human
|
iPSCs (fibroblast-derived)
|
|
Cystic fibrosis
|
Human
|
ESCs
iPSCs (fibroblast-derived; peripheral blood derived)
|
|
HBV infection
|
Human
|
iPSCs (fibroblast-derived)
|
|
Primary liver cancer
|
Human Mouse
|
Adult tissue (surgical resection)
Adult tissue (needle biopsy)
Adult tissue (liver transplantation; genome editing)
Adult tissue (chemical carcinogenesis)
Adult tissue (GEMM)
|
|
Primary sclerosing cholangitis
|
Human
|
Adult tissue (bile-derived; surgical resection)
|
|
Steatosis, steatohepatitis
|
Human Cat
|
iPSCs (fibroblast-derived)
Adult tissue (post-mortem)
|
|
Wilson's disease
|
Dog
|
Adult tissue (surgical resection, needle biopsy, fine needle aspiration)
|
-
Drug Metabolism Simulation: Liver organoids express crucial drug-metabolizing enzymes, including CYP450, allowing for precise evaluation of metabolic rates, active metabolite formation, and potential drug-drug interactions.
-
Early Toxicity Screening: Liver organoids are highly effective in detecting drug-induced liver injury (DILI), identifying key indicators like apoptosis, steatosis, and cholestasis. Notably, they demonstrate superior sensitivity compared to conventional liver cell lines, accurately reflecting clinically relevant toxicities such as acetaminophen hepatotoxicity.
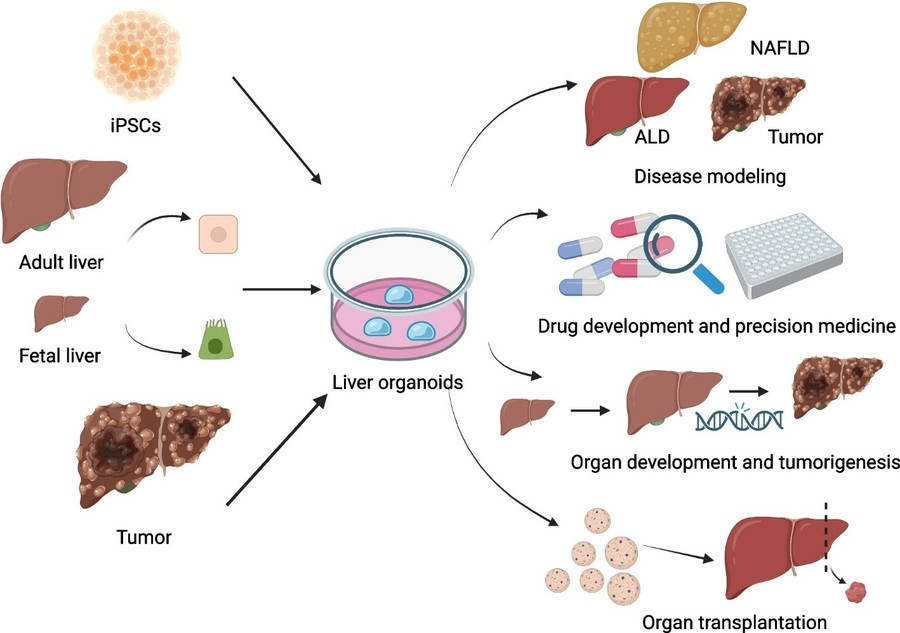 Figure 3 Various applications of liver organoids technology.4,5
Figure 3 Various applications of liver organoids technology.4,5
Regenerative Medicine
Cell transplantation has achieved notable progress across various regenerative medicine applications, yet persistent hurdles remain, such as suboptimal donor material, limited engraftment rates, and the risk of immune rejection. Liver organoid transplantation represents a promising evolution of cellular therapies, offering enhanced therapeutic capabilities. Research consistently indicates that liver organoid transplantation can restore liver function in experimental animal models. For instance, transplanting vascularized human liver organoids into mice with drug-induced liver injury has been shown to successfully improve survival.
Advantages and Disadvantages of Liver Organoids
|
Advantages
|
Disadvantages
|
|
Human-derived: Avoids species-specific biases in drug responses.
|
Incomplete maturation: Limited metabolic enzyme activity compared to adult hepatocytes.
|
|
3D architecture: Mimics cell-cell interactions and zonation.
|
Lack of vascularization: Most models exclude blood vessels, affecting nutrient diffusion.
|
|
Scalability: Suitable for high-throughput drug screening.
|
Cost and complexity: Requires specialized matrices (e.g., Matrigel) and growth factors.
|
|
Patient-specific: Enables precision medicine for rare genetic diseases.
|
Standardization challenges: Variability in protocols across labs.
|
Frequently Asked Questions
Q: What's the main difference between liver organoids and traditional 2D liver cell cultures?
A: The primary difference lies in their dimensionality and complexity. 2D cultures grow cells in a flat layer on a plastic dish, lacking the natural tissue architecture. Liver organoids, however, self-assemble into complex 3D structures that mimic the liver's intricate cellular organization, allowing for more accurate cell-cell interactions and tissue-specific functions.
Q: Are liver organoids actual miniature livers? Can they replace a damaged human liver?
A: While liver organoids remarkably mimic many aspects of the human liver, they are not full miniature organs in the complete sense. They lack full vascularization (blood vessel networks), a complete immune system, and innervation, all of which are crucial for a fully functional organ in vivo. Therefore, they cannot currently replace a damaged human liver for transplantation. Their primary role is as a powerful research tool and potential stepping stone for future regenerative therapies.
Q: What are liver organoids made from?
A: Liver organoids are typically derived from two main sources:
-
Pluripotent Stem Cells (PSCs): These include human embryonic stem cells (hESCs) or induced pluripotent stem cells (hiPSCs). hiPSCs are particularly exciting as they can be generated from a patient's own somatic cells (e.g., skin cells), allowing for patient-specific models.
-
Adult Liver Stem/Progenitor Cells: These are specialized stem cells found within adult liver tissue that retain the capacity to differentiate into various liver cell types.
Q: How long do liver organoids survive in culture?
A: The survival time of liver organoids in culture varies depending on the specific protocol, source cells, and culture conditions. Generally, they can be maintained for several weeks to several months, and in some advanced protocols, even longer, while retaining their functionality.
Conclusion
Liver organoids represent a transformative technology in the field of liver research and medicine. By providing physiologically relevant, human-specific models of liver tissue, they are significantly advancing our understanding of liver development, disease pathogenesis, and drug responses. While challenges remain, particularly regarding complete maturation, vascularization, and immune cell integration, ongoing research is rapidly addressing these limitations. The future holds immense promise for liver organoids to revolutionize drug discovery, personalize patient care, and ultimately contribute to novel therapeutic strategies for a wide range of debilitating liver diseases.
Elevate Your Research with Creative Biolabs' Advanced Liver Organoids Models
Creative Biolabs is at the forefront of biomedical innovation, offering cutting-edge liver organoid services that are transforming drug discovery, disease modeling, and regenerative medicine.
Organoid Models
Organoids Related Products
Creative Biolabs' 3D biology platforms integrate advanced cell culture techniques, microfluidics, and real-time monitoring to deliver physiologically relevant data, bridging the gap between in vitro and in vivo studies. Contact us today to learn more!
References
-
Harrison S P, Baumgarten S F, Verma R, et al. Liver organoids: recent developments, limitations and potential. Frontiers in medicine, 2021, 8: 574047. https://doi.org/10.3389/fmed.2021.574047
-
Chen Y, Liu Y, Chen S, et al. Liver organoids: a promising three-dimensional model for insights and innovations in tumor progression and precision medicine of liver cancer. Frontiers in Immunology, 2023, 14: 1180184. https://doi.org/10.3389/fimmu.2023.1180184
-
Nuciforo S, Heim M H. Organoids to model liver disease. JHEP Reports, 2021, 3(1): 100198. https://doi.org/10.1016/j.jhepr.2020.100198
-
Sang C, Lin J, Ji S, et al. Progress, application and challenges of liver organoids. Clinical Cancer Bulletin, 2024, 3(1): 7. https://doi.org/10.1007/s44272-024-00012-0
-
Distributed under Open Access license CC BY 4.0, without modification.
Research Model
Related Sections:

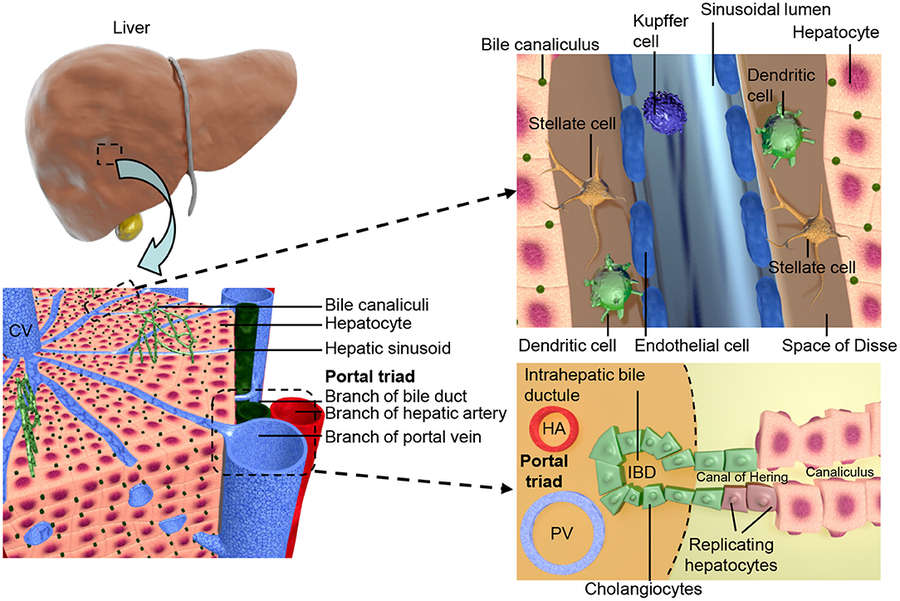 Figure 1 Shows the structural organization of the liver at different scales.1,5
Figure 1 Shows the structural organization of the liver at different scales.1,5
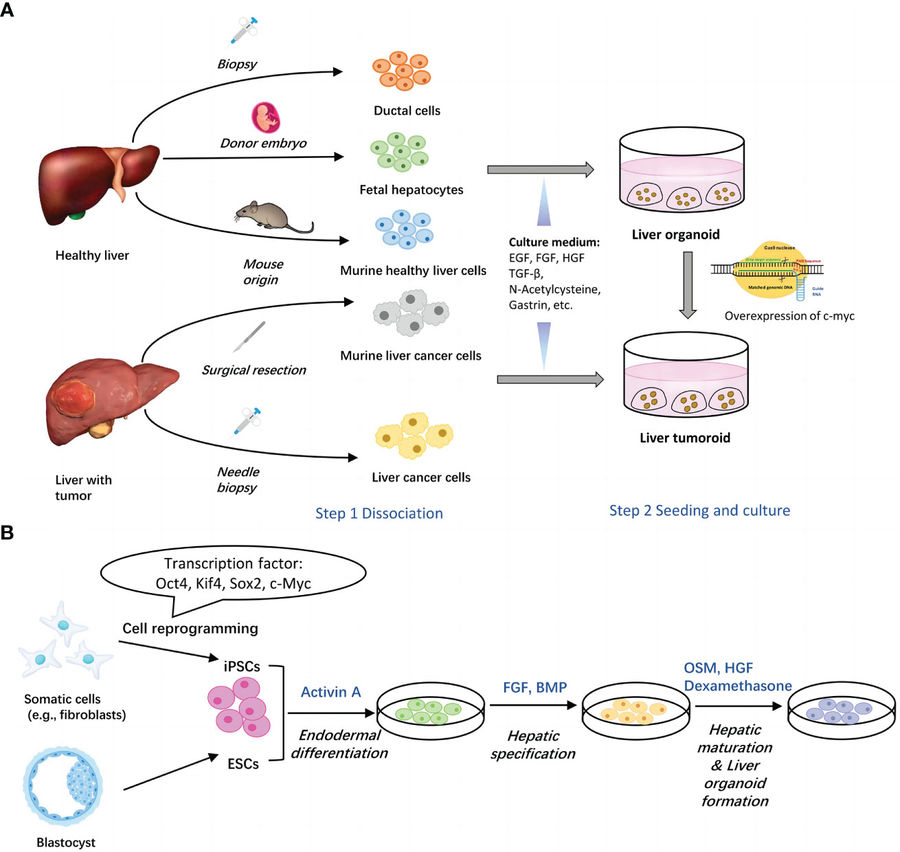 Figure 2 Two main methods for generation of liver organoids.2,5
Figure 2 Two main methods for generation of liver organoids.2,5
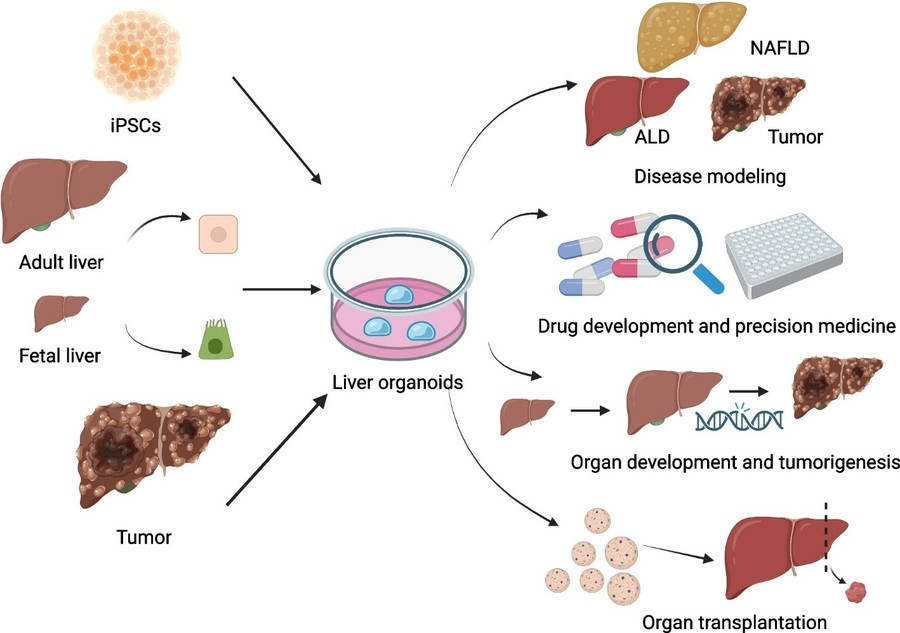 Figure 3 Various applications of liver organoids technology.4,5
Figure 3 Various applications of liver organoids technology.4,5