Klinefelter Syndrome
Klinefelter syndrome (KS) is a genetic disorder related to chromosomal abnormalities that primarily affects males, resulting in an extra X chromosome. KS stands as the most common sex chromosome aneuploidy in males, with an estimated incidence of 1 in 500 to 1 in 1000 live births. The additional X chromosome stems from a nondisjunction event during meiosis, which can occur in either the paternal or maternal gamete. KS follows an X-linked recessive inheritance pattern, indicating that males who inherit the extra X chromosome from their mothers are affected, while females who inherit it from their fathers become carriers. Risk factors for KS encompass advanced maternal age, paternal age, and environmental factors such as exposure to radiation or chemicals. KS presents as a heterogeneous disorder, leading to various phenotypic manifestations and health implications for affected individuals.
Clinical Features
KS is a heterogeneous disorder with diverse phenotypic manifestations and health implications for those affected. The clinical features can be categorized into typical and atypical features based on their frequency and severity. Typical features are present in most or all cases, whereas atypical features occur in some or a few cases.
Table 1. The typical and atypical features of KS
| System | Typical features | Atypical features |
| Reproductive | Small, firm testicles; low or absent sperm count; infertility; small penis; undescended testes | Hypospadias; micropenis; cryptorchidism |
| Endocrine | Low testosterone levels; low sex drive; gynecomastia; increased abdominal fat | Diabetes mellitus; metabolic syndrome; thyroid dysfunction |
| Neurological | Learning disabilities; speech delay; dyslexia; attention deficit hyperactivity disorder (ADHD); autism spectrum disorder (ASD) | Seizures; tremors; Parkinson’s disease |
| Cardiovascular | Varicose veins; deep vein thrombosis (DVT); pulmonary embolism (PE) | Congenital heart defects; mitral valve prolapse; aortic aneurysm |
| Skeletal-muscular | Tall stature; long legs; short torso; broad hips; osteoporosis; osteoarthritis | Scoliosis; joint hypermobility |
| Immune | Autoimmune diseases (eg, systemic lupus erythematosus, rheumatoid arthritis, Sjögren’s syndrome) | Increased susceptibility to infections |
| Psychiatric-behavioral | Shyness; social anxiety; low self-esteem; depression; mood swings | Aggression; impulsivity; substance abuse |
The clinical features of KS may vary depending on the karyotype, the degree of mosaicism, the age of diagnosis, and the individual's treatment status. Some features may manifest at birth or during childhood, while others may emerge during puberty or adulthood. These clinical features can impact the individual's quality of life and social adaptation, leading to challenges in education, employment, relationships, and mental health. Therefore, early diagnosis and intervention are crucial for improving outcomes and the well-being of individuals with KS.
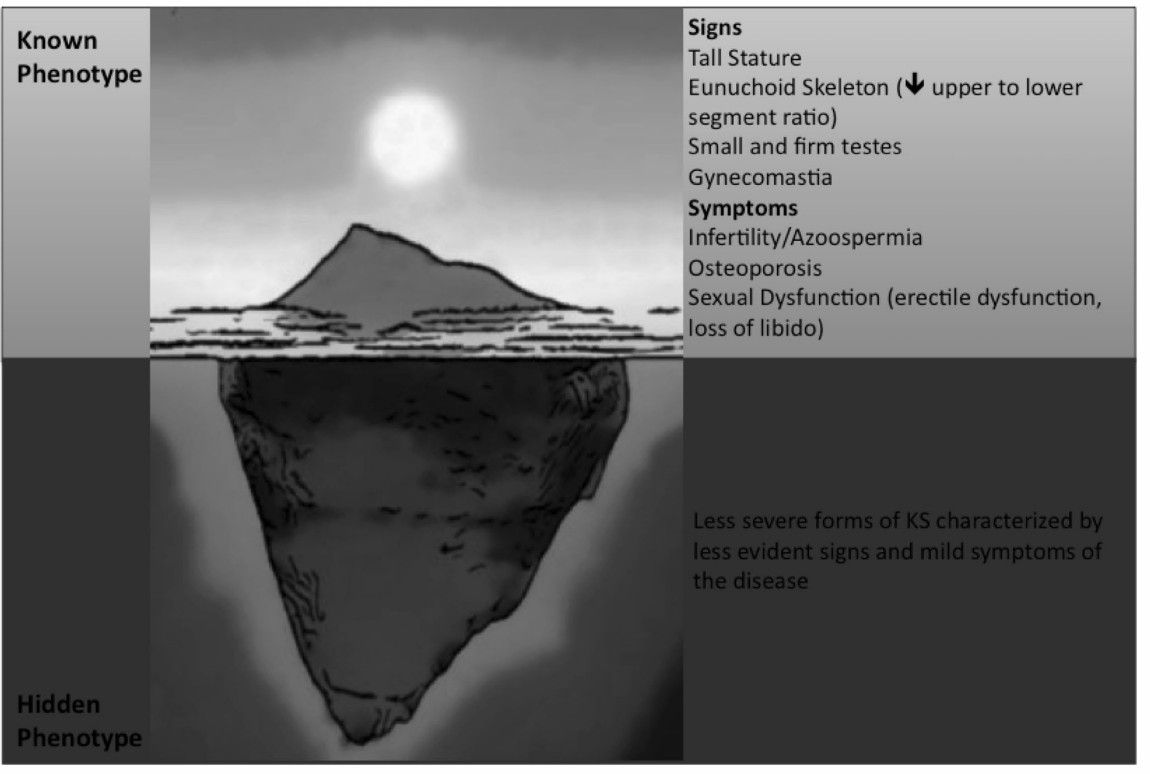 Fig.1 Signs and symptoms of KS according to the severity of clinical phenotype. (Bonomi M, 2017)
Fig.1 Signs and symptoms of KS according to the severity of clinical phenotype. (Bonomi M, 2017)
Clinical Diagnosis and Treatment Method
KS is diagnosed through hormone testing and chromosome analysis, which reveal abnormal hormone levels and an extra X chromosome in blood samples. Prenatal testing methods such as amniocentesis or chorionic villus sampling can also detect KS before birth. Treatment aims to minimize the physical, mental, and reproductive health effects of KS. Options include testosterone replacement therapy, breast tissue removal, speech and physical therapy, educational evaluation and support, and reproductive assistance. Testosterone replacement therapy enhances various aspects of physical and mental health, while breast tissue removal reduces gynecomastia. Speech and physical therapy improve communication skills, motor skills, coordination, and posture. Educational evaluation and support assess and assist learning and socialization abilities. Reproductive assistance offers infertile men a chance at fatherhood through advanced reproductive technologies like sperm retrieval and intracytoplasmic sperm injection (ICSI).
Summary and Outlook
Klinefelter syndrome is a common but often underdiagnosed condition that warrants increased attention and awareness from the medical community and the public. Further research is necessary to comprehend the pathogenesis, epidemiology, natural history, and long-term consequences of KS. Studies should also evaluate the efficacy and safety of different treatment modalities and explore new therapeutic options and strategies. Additionally, efforts should focus on providing better education, counseling, and support for individuals with KS and their families, promoting their social integration and acceptance. With proper diagnosis and treatment, Klinefelter syndrome should not hinder individuals from achieving a fulfilling life; they can overcome challenges and realize their full potential.
References
- Bonomi M, et al. Klinefelter syndrome (KS): genetics, clinical phenotype and hypogonadism. J Endocrinol Invest. 2017 Feb;40(2):123-134.
