Candida glabrata
Candida spp. is the leading opportunistic fungal pathogen that leads to infections in humans, ranging from superficial mucosal lesions to disseminated or bloodstream candidiasis. Although Candida infections exist with high frequency, there is a limited number of antifungal drugs available for treatment. Antifungal drug discovery services team at Creative Biolabs now delivers the highest quality, full-service contract research to support the pharmaceutical and biotechnology sectors. Here, we focused on the Candida glabrata.
Introduction to Candida Glabrata
Candida glabrata (C. glabrata), which is previously known as Torulopsis glabrata, is a haploid yeast of the genus Candida. C. glabrata is distinguished by blastoconidial morphology and haploid genome when contrasts with other Candida species. With the increasing population of immunocompromised individuals, C. glabrata has been shown to be a highly opportunistic pathogen of the urogenital tract, and of the bloodstream (known as Candidemia). Currently, it ranks second or third as the causative microorganism of superficial (oral, esophageal, urinary, or vaginal) and systemic candidal infections, which are often nosocomial. Infection of C. glabrata is especially prevalent in the elderly and HIV positive people.
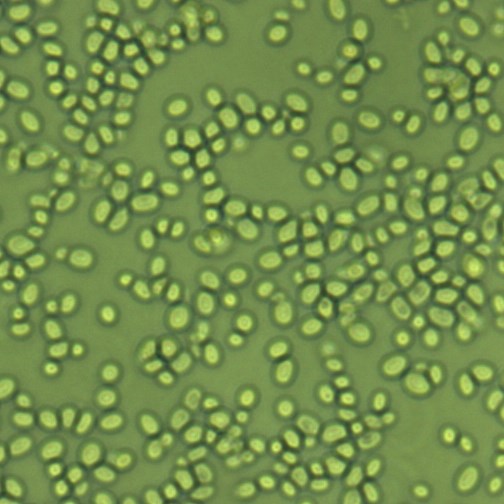 Fig.1 Candida glabrata. Distributed under CC BY-SA 4.0, from Wiki, without modification.
Fig.1 Candida glabrata. Distributed under CC BY-SA 4.0, from Wiki, without modification.
Pathogenesis of C. Glabrata
Two potential virulence factors have been widely cited to play a role in the pathogenicity of C. glabrata. The first is an array of adhesins coded by the epithelial adhesin (EPA) genes. The EPA gens can respond to environmental signals which allow them to be expressed abundantly so that C. glabrata. can adhere to biotic and abiotic surfaces in microbial mats. This is also supposed to be the possible mechanism by which C. glabrata forms microbial "biofilms" on urinary catheters and less commonly in-dwelling IV catheters. In addition, the inflammation of the gut changes the microbial balance in the human body and result in remodeling of C. glabrata cell wall by an increase in chitin, which contributes to promoting persistence of C. glabrata in the gut.
Antifungal Drugs Against C. Glabrata
A major phenotype and potential virulence factor that C. glabrata has is low-level intrinsic resistance to the azole drugs, which are the most commonly used antifungal agents. Thus, treatment of C. glabrata infections can include azoles but often needs flucytosine or polyene drugs, such as amphotericin B and nystatin. Intravenous delivery of amphotericin B is a therapeutic method of last resort, leading to other side effects, such as chronic renal failure.
Antifungal Drug Discovery Services Against C. Glabrata at Creative Biolabs
As a world leading CRO service provider, the antifungal drug discovery services team at Creative Biolabs provides the highest quality, full-service contract research to assist you in preclinical antifungal drug development. Our services in this field range from target identification and validation, Hit identification, Hit to lead, to Lead optimization and IND enabling.
You may also be interested in other fungi that may be implicated in candidiasis:
Aided by the world-class technology and advanced facilities, scientists at Creative Biolabs devote themselves to providing the most comprehensive series of antifungal drug discovery services for our worldwide clients. Please contact us for more details or technical support.
For Research Use Only.
