Oncolytic Virus Biodistribution Study Service
When an oncolytic virus (OV) is introduced into the body, it is essential to study its biodistribution characteristics. In the context of clinical treatment, the most efficacious route of drug administration, as well as the optimal dosage and dosing frequency, can be determined by elucidating its in vivo distribution, thereby circumventing potential toxic side effects. Moreover, the biodistribution findings of oncolytic viruses can guide genetic engineering efforts to enhance the viruses' targeting ability and tumor specificity. Additionally, based on their distribution characteristics, rational combined treatment strategies can be designed to potentiate the anti-tumor immune response and improve the therapeutic outcome.
The Biodistribution Characteristics of OV
The biodistribution of oncolytic viruses within the body is intricate and influenced by a multitude of factors.
Biodistribution of the OV at the beginning of infection
- During intratumoral injection, the OVs initially accumulate in large quantities within the local tumor mass. Subsequently, it spreads rapidly throughout the tumor parenchyma, directly infecting tumor cells.
- When OVs are given via local injection routes like intramuscular or subcutaneous injection, they first spread in adjacent tissues at the injection site, potentially infecting nearby fibroblasts, macrophages, etc. Later, some of the virus may start migrating to the draining lymph nodes through the local lymphatic network.
- When OVs are intravenously administered, they enter the bloodstream and spread throughout the systemic circulation. A part of the virus gets cleared within minutes to hours. Only a small amount remains in the bloodstream and is carried to the capillary beds of tissues and organs.
Biodistribution of the OV in the middle and late stages of infection
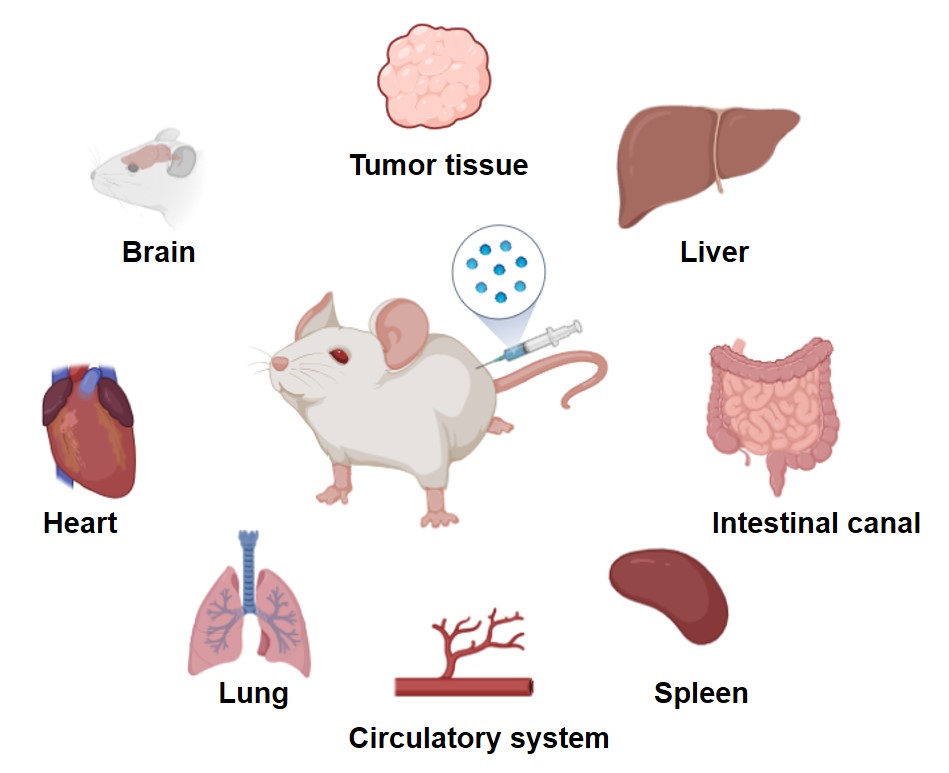
Tumor Tissue
Ideally, oncolytic viruses should concentrate highly in tumor tissue. Tumors' unique physiological traits, such as abnormal angiogenesis with wide-gap blood vessel walls, allow virus extravasation. Moreover, overexpressed viral receptors on tumor cells promote virus binding and infection.
Liver
Kupffer cells in the liver can recognize and uptake viral particles in the bloodstream. Surface proteins/structures of some oncolytic viruses (e.g., adenoviruses) bind to specific liver cell receptors (e.g., CAR), causing virus distribution in the liver.
Lung
The virus readily reaches the lungs via the bloodstream. Additionally, the respiratory mucosa may be exposed to oncolytic viruses (for instance, during inhalation-based administration). Once within the lungs, the virus is capable of infecting alveolar epithelial cells and pulmonary macrophages.
Kidney
Oncolytic virus particles in the circulation may pass through the glomerular filtration and enter the renal tubules, with some of the virus being excreted in the urine.
Assays for the Biodistribution of OVs
Oncolytic viruses can be labeled using radiolabeled, fluorescent, or bioluminescent techniques. In vivo imaging systems such as positron emission tomography (PET), single-photon emission computed tomography (SPECT), fluorescence imaging, or bioluminescence imaging are then employed. Through these methods, the distribution, dynamic alterations, and metabolic processes of the virus in different tissues and organs of animals can be observed, enabling an understanding of the virus's targeting ability and clearance rate in vivo.
Tab.1 Common method for oncolytic virus biodistribution studies.
| Labeling of Viruses | Sample Collection and Detection |
|---|---|
| Radionuclide labeling: Radionuclides such as iodine-125 or technetium-99m are used to label oncolytic viruses. By employing SPECT or PET techniques for detection, the distribution of the virus in animals can be tracked in real time. This approach offers high sensitivity. | Tissue homogenization method: Animal tissues and organs are collected and homogenized, and the virus content is determined by radioactive counting, fluorescence detection, or enzyme-activity-based assays. |
| Fluorescent labeling: Oncolytic viruses are labeled with fluorescent dyes or fluorescent proteins such as GFP and RFP. Fluorescence signals are observed via fluorescence microscopy or in vivo imaging systems. This technique is relatively straightforward to perform, yet the signals may be disrupted by tissue auto-fluorescence. | Immunohistochemical method: Specific antibodies against oncolytic virus structural proteins or marker proteins are used for immunohistochemical staining. This allows the observation of virus distribution in tissue sections, providing a more intuitive visualization. |
| Bioluminescence labeling: A bioluminescent reporter gene, such as the luciferase gene, is introduced into the virus. After the addition of the luciferin substrate, the distribution of the virus in vivo is detected using a bioluminescence imaging system. This approach exhibits high sensitivity and specificity. | In situ hybridization: Specific probes for the viral genome are designed to carry out in situ hybridization experiments to detect the presence and distribution of viral nucleic acids. |
