Disease Specific Oncolytic Virotherapy Development Services
Difficulties in Treatment Oncolytic Mechanism Related Sections
Cancer is a type of harmful tumor that starts when cells grow abnormally. Without the normal controls that keep cell growth in check, cancer cells multiply, spread, and invade other tissues. Many things can cause cancer, including physical factors, chemicals, germs, and genes.
Old-fashioned treatments like surgery, chemotherapy, and radiation can help, but they don't work perfectly. Surgery can't always get rid of tiny cancer cells that have spread. Chemo and radiation can also hurt healthy cells, which leads to bad side effects. That's why we need new and better ways to treat cancer.
The Difficulties in The Process of Tumor Treatment
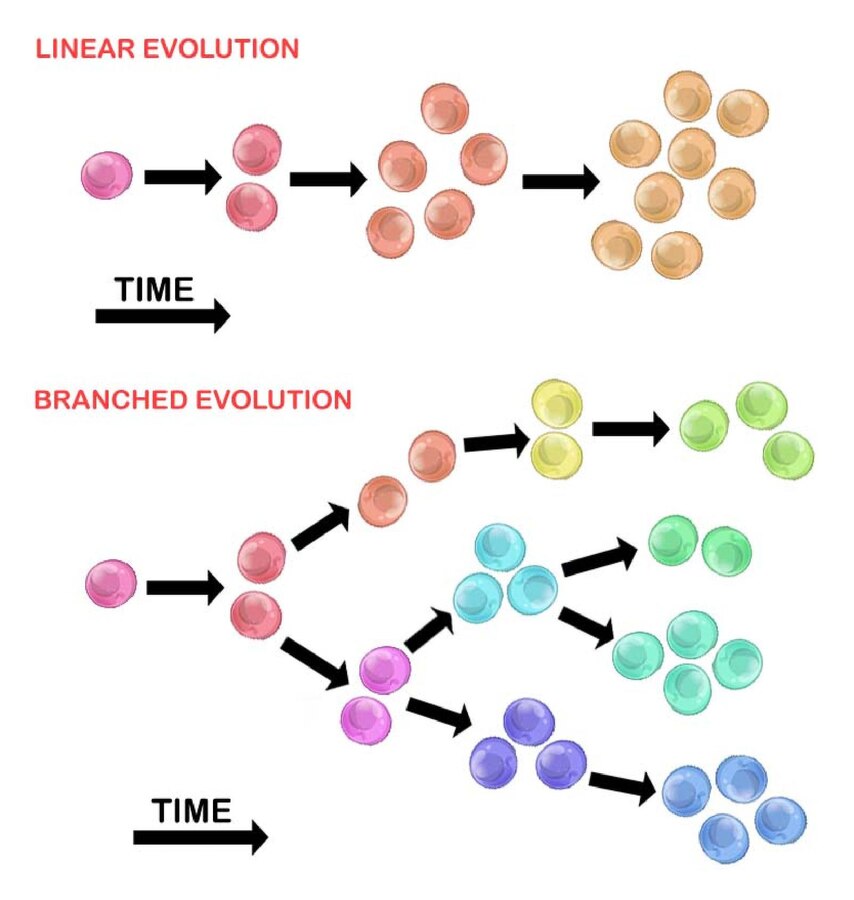
- Tumor heterogeneity
 Distributed under CC BY-SA 3.0, from Wiki, without modification.
Distributed under CC BY-SA 3.0, from Wiki, without modification.
Tumor cells mutate during growth, causing disparities in genes, metabolism, and drug sensitivity. This makes single-target therapies ineffective, leading to recurrence. For example, breast cancer has diverse molecular subtypes like Luminal A, B, HER2-overexpressing, and triple-negative. Each subtype responds differently to treatment and prognosis. Also, tumor cells may vary between primary and metastatic sites in the same patient.
 Distributed under CC 1.0, from Wiki, without modification.
Distributed under CC 1.0, from Wiki, without modification.
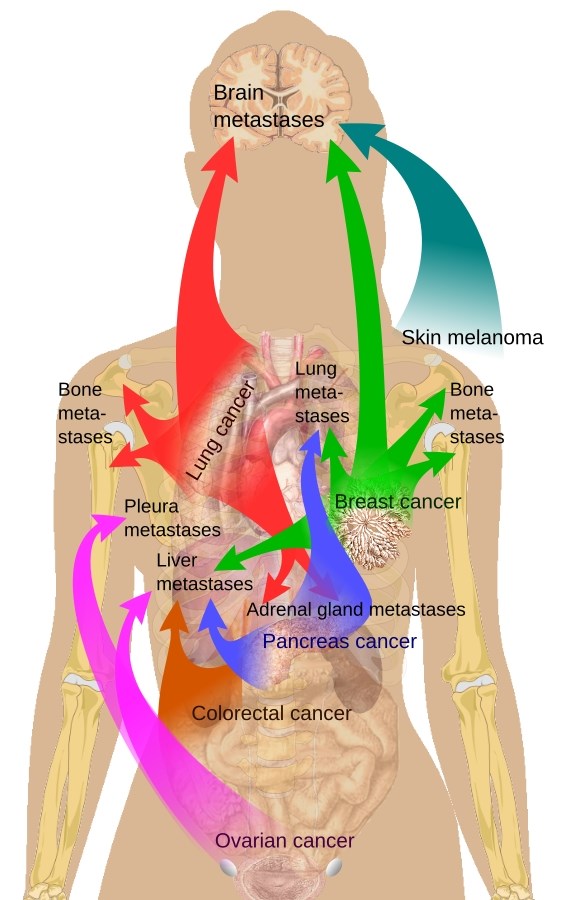
- Tumor invasion and metastasis
Tumor cells can invade and spread. They can travel to other parts of the body through the blood or lymph vessels and form new tumors in far-off places. For example, lung cancer cells often spread to important organs like the brain, bones, and liver. When these new tumors form, it not only stops those organs from working properly but also limits the treatments that doctors can use.
- Side effects of treatment
Traditional chemo-and radiotherapy, while eradicating tumor cells, harms normal cells and tissues, triggering severe side effects. Chemotherapy drugs often impact bone marrow hematopoiesis and induce gastrointestinal reactions. Radiotherapy causes local radiation damage. These side effects degrade patient quality of life, potentially forcing treatment adjustments and compromising efficacy.
- Drug resistance
Giving chemotherapy drugs or targeted molecular treatments continuously during cancer treatment often leads to tumor cells becoming resistant to the drugs. A good example is chronic myeloid leukemia. Some patients, after being treated for a long time, stop responding to tyrosine kinase inhibitors (TKIs), and this causes their condition to get worse.
The Oncolytic Mechanism of Oncolytic Viruses
- Direct lysis of tumor cells
OVs are capable of inserting cell or tissue-specific promoters, which enables enhanced attachment to the tumor cell membrane. They can replicate and proliferate by exploiting host resources and ultimately lyse host cells to exert anti-tumor effects. Nevertheless, OVs are unable to infect every tumor cell within the body.
- Activation of anti-tumor immune responses
OVs are highly effective in inducing antitumor immune activity. Viral infection leads to the local release of soluble tumor-associated antigens, cell-derived DAMPs, and viral PAMPs. These can be recognized and captured by APCs. By generating inflammation within the tumor, OVs promote both innate and adaptive immunity. In this way, OVs disrupt the immune tolerance to tumor antigens and can even elicit tumor-specific memory responses.
- Disruption of the vasculature in the tumor
Under hypoxic conditions, the profusion of angiogenic factors within the tumor microenvironment instigates the recruitment of blood vessels. Oncolytic viruses can be activated by EGFR/Ras pathway signaling, cellular TK levels, and cancer cells' resistance to IFN-Ⅰ. These activated OVs can induce the formation of neutrophil aggregates in blood vessels. The neutrophil aggregates initiate fibrin deposition and release coagulation factors, ultimately leading to the disruption of tumor blood vessels.
- Induction of apoptosis and arrest of cell cycle
Furthermore, OVs can trigger immunogenic apoptosis, necroptosis, pyroptosis, and autophagic cell death. OVs not only have the capacity to induce necroptosis in tumor cells but can also activate anti-tumor immunity through the Gasdermin family (GSDM). Additionally, OVs can be genetically engineered to express cell-cycle-related cytokines, thereby acquiring the ability to arrest the cell cycle.
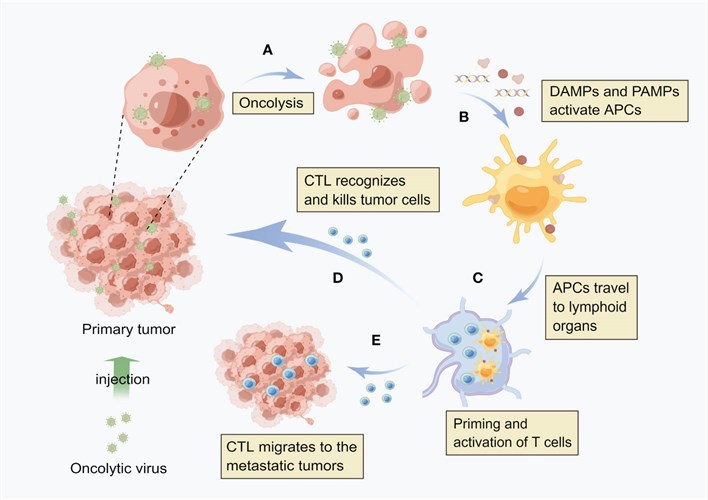 Fig.1 Oncolytic viruses induce local and systemic antitumor immunity.1
Fig.1 Oncolytic viruses induce local and systemic antitumor immunity.1
With the continuous progress of genetic engineering and virus-engineering technologies, oncolytic virus therapy holds great promise. Creative Biolabs relies on a stable platform to enhance the construction efficiency of a variety of viral vectors and can further engineer a variety of viruses according to customer requirements. After construction, a series of in vitro experiments are to be performed to assess viral replication capacity, cytotoxic efficacy, and the expression and functional characteristics of the transgene. At the same time, a comprehensive and reasonable in vivo study plan is to be developed to fully verify the therapeutic effect of oncolytic viruses through experiments in relevant disease models.
Reference
- Zhu, Licheng, et al. "Recent advances in oncolytic virus therapy for hepatocellular carcinoma." Frontiers in oncology 13 (2023): 1172292. DOI: 10.3389/fonc.2023.1172292. Distributed under Open Access license CC BY 4.0, without modification.
