Introduction What We Can Offer? Why Choose Us? FAQs Related Products Services
Accelerate Your Research and Development!
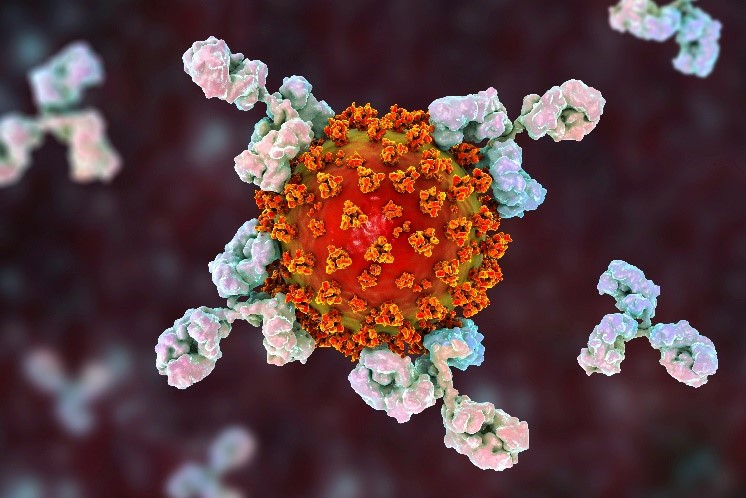
The complement system is a vital component of the innate immune response, acting as a crucial first line of defense against pathogens. Are you currently facing challenges in developing effective anti-infective therapies or understanding complex host-pathogen interactions? Creative Biolabs' Complement System Therapeutic services help you accelerate drug discovery and develop highly specific antibodies and inhibitors to modulate this critical pathway through our advanced protein engineering and high-throughput screening platforms.
Contact our team to get an inquiry now!
Introduction
The complement cascade constitutes an intricate assembly of over 30 plasmatic and membrane-bound proteins functioning as a cornerstone of innate immunity. Its designation "complement" originates from its capacity to potentiate antibody and phagocyte activities in eliminating pathogens and compromised cells. Activation occurs through three principal routes—classical, lectin, and alternative—all culminating in C3 convertase formation. This enzyme cascade leads to three key outcomes: opsonization (marking pathogens for phagocytosis), direct cell lysis via the formation of the membrane attack complex (MAC), and the generation of pro-inflammatory signals.
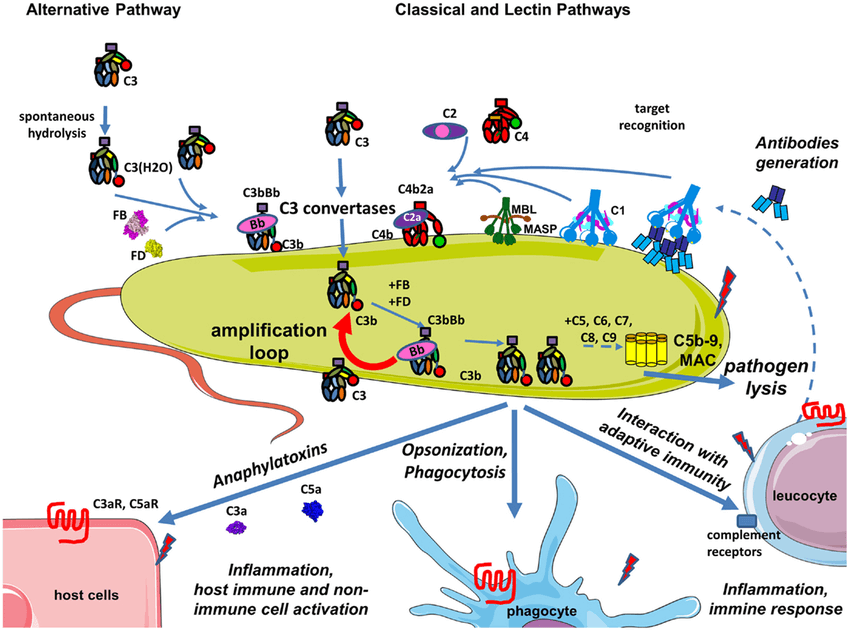 Fig.1 Complement during infection with a pathogen.1
Fig.1 Complement during infection with a pathogen.1
In the context of infection, the complement system serves as a rapid-response mechanism. It can directly recognize and bind to foreign surfaces on pathogens without prior exposure, initiating a cascade that leads to their destruction. For example, complement proteins can opsonize bacteria, making them more susceptible to engulfment and killing by phagocytes. This process is essential for controlling the spread of infections. However, many pathogens have evolved sophisticated strategies to evade or hijack the complement system, highlighting the need for targeted therapeutic interventions.

Specific Infectious Diseases and Conditions
Our focus on the complement system is directly applicable to a range of critical infectious diseases and related conditions. By targeting or modulating this pathway, we can help develop novel therapies for:
-
Recurrent Infection: Linked to complement deficiencies, our therapies can replace or bypass defective proteins.
-
Septic Shock: We develop solutions that inhibit specific complement factors to mitigate the overwhelming inflammatory response in severe sepsis.
-
Meningococcal Meningitis: Our approaches enhance the lytic activity of the complement cascade to clear Neisseria meningitidis.
-
Primary Amebic Meningoencephalitis (PAM): Our services support therapies that block complement evasion mechanisms used by pathogens like Naegleria fowleri.
-
Chemotherapy-induced Neutropenia: For immunocompromised patients, we develop therapies that enhance complement activity to serve as a critical defense line.
Physiological Roles of Complement in Infectious Diseases
The complement system is a critical part of the innate immune response, providing immediate defense and debris clearance. Its activation results in several outcomes that directly combat infection:
-
Opsonization: Complement fragments coat pathogens, making them "sticky" and easier for phagocytic cells to destroy.
-
Direct Lysis: The Membrane Attack Complex (MAC) forms pores in certain pathogens' membranes, causing them to burst.
-
Chemotaxis: Complement fragments recruit immune cells to the infection site.
-
Inflammation: These fragments trigger local inflammation to create a hostile environment for pathogens.
-
Clearance of Immune Complexes and Apoptotic Cells: The system tags and helps clear dead cells and immune complexes, preventing chronic inflammation.
What We Can Offer?
To help you advance your research and development, Creative Biolabs provides a comprehensive suite of products and services for complement system therapeutics. Our offerings are designed to support every stage of your drug discovery journey, from initial target identification to preclinical validation.
Our services include:
-
Complement-Dependent Cytotoxicity (CDC) Assay: A highly accurate functional assay to evaluate the ability of therapeutic antibodies to induce complement-mediated cell lysis.
-
Therapeutic Antibody and Inhibitor Development: Development of highly specific monoclonal antibodies and inhibitors.
-
Recombinant Complement Proteins: High-purity proteins for research and assay development.
-
Functional Assay Services: A full portfolio of complement activation and inhibition assays, including CH50/AP50, C3/C4 deposition, and hemolytic assays.
-
Complement Evasion Studies: Services to evaluate how pathogens evade the complement system and to develop strategies to overcome these mechanisms.
Why Choose Us?
Choosing a partner for complement therapeutic development requires deep expertise and robust technology. Creative Biolabs’ unique blend of scientific knowledge and commitment to superior results sets us apart. Our experienced team leverages proprietary platforms and advanced assays to create customized molecules and ensure the highest quality standards. This is reflected in published data that demonstrates the efficacy and specificity of our developed products.
Our key advantages include:
-
Deep Scientific Expertise: A team with extensive knowledge of the complement cascade.
-
Advanced Platforms: Cutting-edge technology for high-throughput screening, protein production, and functional assays.
-
Customization: Flexible service models tailored to your project.
-
Rapid Turnaround: Optimized workflows to accelerate your research.
-
Exceptional Quality: Stringent quality control at every stage.
Access the Creative Biolabs Benefit - Request a Quotation Now
FAQs
Q: How does regulating the complement cascade combat pathogens?
A: By either enhancing the body's natural complement response to target pathogens more effectively or, conversely, by inhibiting excessive or misdirected complement activation that can cause host tissue damage during an infection. The goal is to fine-tune the immune response for a more favorable outcome.
Q: Can therapeutic antibodies against complement components be used for any type of infection?
A: The application depends on the specific pathogen and its interaction with the complement system. Some antibodies may be highly effective against pathogens that are particularly susceptible to complement-mediated lysis, while others might be designed to reduce inflammation in a host. A detailed understanding of the mechanism is crucial.
Q: What are the risks of inhibiting the complement system for therapeutic purposes?
A: The primary risk is a potential increase in susceptibility to certain infections, particularly those caused by encapsulated bacteria. Therefore, targeted inhibition that spares the overall protective function of the system is key.
Q: How do you validate the efficacy of a therapeutic candidate that targets the complement system?
A: We use a combination of in vitro and in vivo assays. This includes functional tests to measure complement activation, binding assays to confirm target specificity, and cell-based assays to evaluate their biological effect. These rigorous methods ensure your candidate performs as expected.
Q: Is it possible to develop a therapeutic that targets only a specific pathway of the complement system?
A: Yes, it is. The complement system has three distinct activation pathways, and therapeutics can be designed to block one or more of them. This allows for a more precise intervention, avoiding broad-spectrum effects that could compromise the host's overall immune defense.
Creative Biolabs is your trusted partner in harnessing the power of the complement system for therapeutic innovation. Our comprehensive services, from antibody development to functional assays, and our specialized focus on diseases, are designed to accelerate your project and lead you to successful outcomes.
Related Hot Products
Click Here to Explore Our Full Product Catalog
Related Hot Services
Click Here to Explore Our Advanced Complement Therapeutics Platform
Reference
-
Merle, Nicolas S et al. "Complement System Part I - Molecular Mechanisms of Activation and Regulation." Frontiers in Immunology vol. 6 262. 2 Jun. 2015, Distributed under Open Access license CC BY 4.0, without modification. https://doi.org/10.3389/fimmu.2015.00262
For Research Use Only.
Related Sections:

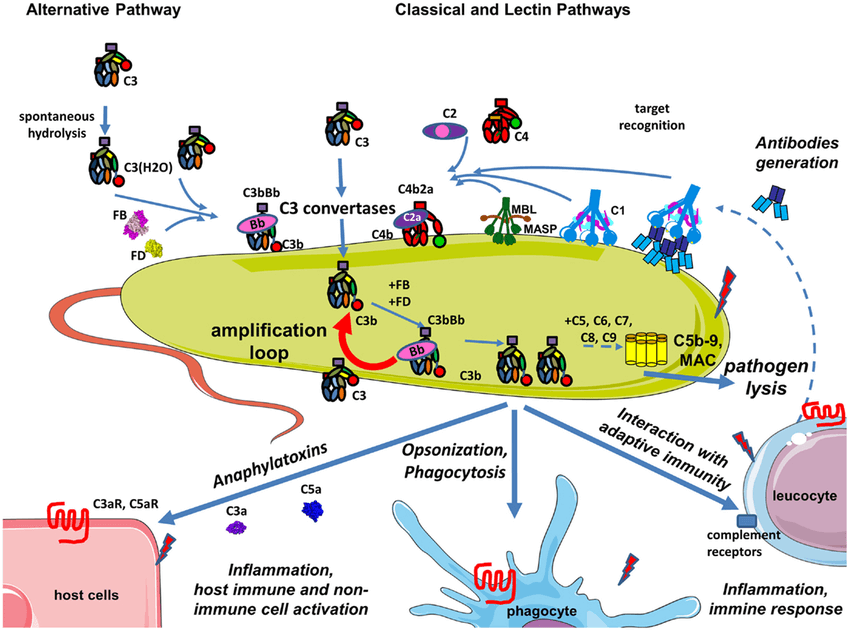 Fig.1 Complement during infection with a pathogen.1
Fig.1 Complement during infection with a pathogen.1