Introduction What We Can Offer? Why Choose Us? FAQs Featured Services Featured Products
Accelerate Your Research and Development!
Are you currently facing long drug development cycles for ocular diseases, difficulty in targeting specific complement pathways, or challenges in developing effective Age-Related Macular Degeneration (AMD) treatments? Creative Biolabs' Complement System Therapeutic solutions help you accelerate AMD therapeutic discovery, obtain highly specific complement inhibitors, and streamline preclinical development through advanced antibody engineering, high-throughput screening, and innovative complement modulation techniques.
Contact our team to get an inquiry now!
Introduction
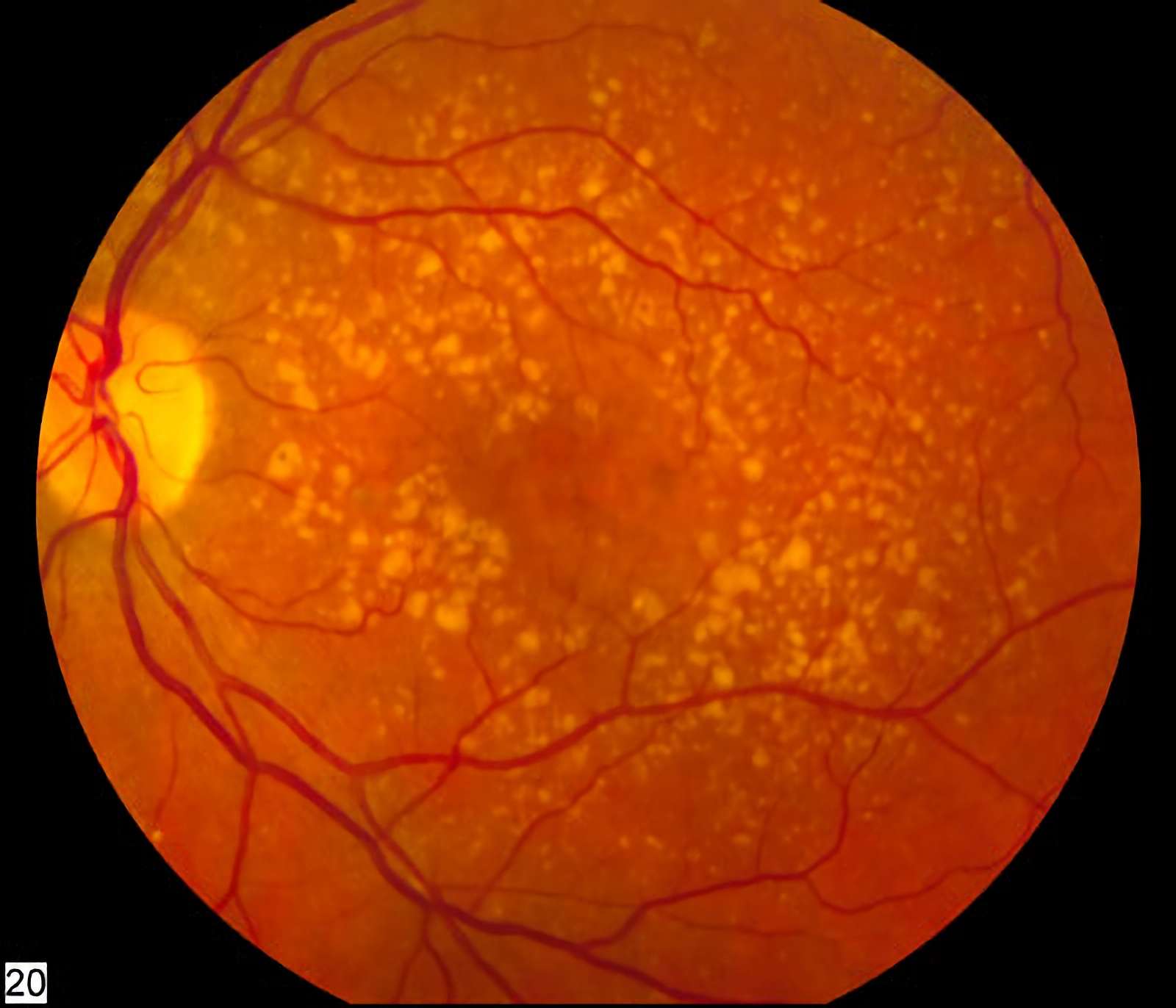
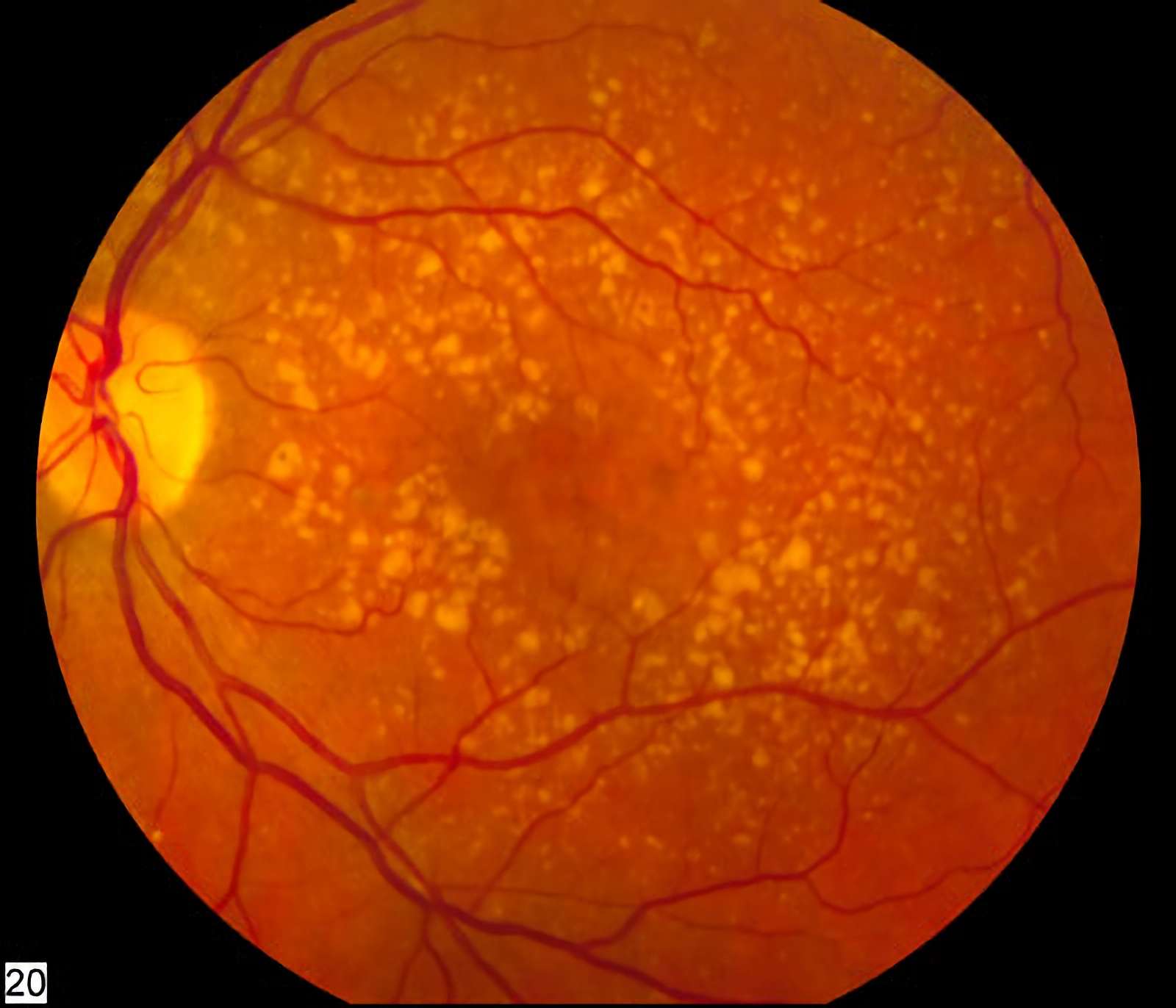
Age-related Macular Degeneration (AMD) is a leading cause of irreversible vision loss among the elderly, characterized by progressive damage to the macula, the central part of the retina responsible for sharp, detailed vision. AMD manifests in two primary forms: dry (atrophic) AMD, accounting for 85-90% of cases, involves the gradual thinning of the macula and the formation of drusen (yellowish deposits of extracellular material); and wet (neovascular) AMD, characterized by abnormal blood vessel growth under the retina, leading to fluid leakage, hemorrhage, and rapid vision loss. The pathogenesis of AMD is multifactorial, involving genetic predispositions, environmental factors, and chronic inflammation.
 Distributed under Open Access license CC BY-SA 4.0, from Wiki,
without modification.
Distributed under Open Access license CC BY-SA 4.0, from Wiki,
without modification.
Fig.1 Intermediate age related macular degeneration.
AMD Genetic Risk Factor
Several genetic variants that influence susceptibility to AMD have recently been identified. Individuals who’s already had one or more of these genetic variations are at particularly high risk of developing AMD if they also smoke. The gene related to AMD is shown below.
|
Complement factor H
|
ATP-binding cassette transporter
|
Collagen type 8 alpha 1 subunit
|
|
Vascular endothelial growth factor A
|
Complement factor B
|
Fyn-related kinase/alpha chain of type X collagen
|
|
HtrA-serinepeptidase1
|
Hepatic lipase
|
Cholesterylester transfer protein
|
|
Complement factor 1
|
Apolipoprotein E
|
Tissue inhibitor of metalloproteinase 3
|
|
Complement component 3
|
Complement component 2
|
Tumour necrosis factor receptor superfamily 10a
|
What We Can Offer?
Creative Biolabs provides a comprehensive range of products and services designed to facilitate the research and development of complement system therapeutics for Age-Related Macular Degeneration:
-
Recombinant Complement Proteins: High-quality, functionally active recombinant complement factors and regulatory proteins for research and assay development.
-
Anti-Complement Factor Antibodies: A diverse catalog of highly specific antibodies targeting various complement components (e.g., C3, C5, Factor B, Factor D, Factor H) for research, diagnostic, and therapeutic development purposes.
-
Complement Pathway Functional Assays: Development and execution of robust in vitro and cell-based assays to evaluate complement activation, inhibition, and pathway-specific modulation.
-
Complement Inhibitor Screening Services: High-throughput screening platforms for the identification of novel small molecule or biologic inhibitors of complement activation.
-
Antibody Engineering and Optimization: Services for the design, engineering, and optimization of therapeutic antibodies, including humanization, affinity maturation, and specificity enhancement.
Why Choose Us?
Creative Biolabs stands at the forefront of complement system therapeutic development for AMD, offering unparalleled expertise and cutting-edge platforms. Our commitment to scientific rigor and client success sets us apart.
-
Sophisticated Technology Platforms: We utilize cutting-edge tools for automated screening, antibody refinement, and functional test design, guaranteeing identification and enhancement of maximally effective complement-targeting inhibitors.
-
End-to-End Service Solutions: Spanning target discovery/verification through lead refinement and preclinical analysis, we provide a comprehensive workflow supporting complete AMD therapeutic development pipelines.
-
Proven Track Record: Our methodologies have consistently yielded promising therapeutic candidates and insights. (Published Data indicate our success in identifying novel modulators of complement activity.)
-
Personalized Approaches: We appreciate every initiative's distinctive requirements. Our flexible approach allows us to tailor our services to meet your specific research objectives and timelines, ensuring maximum efficiency and relevance.
-
Quality and Reliability: Adherence to stringent quality control measures at every stage of development guarantees the reliability and reproducibility of our data and deliverables.
Obtain the Creative Biolabs Advantage – Request Details Immediately
FAQs
Q: How can targeting the complement system specifically impact the progression of AMD?
A: Modulating specific components of the complement cascade can help mitigate the chronic inflammation and cellular damage that drive AMD progression. By inhibiting key activation points or enhancing regulatory mechanisms, it's possible to reduce drusen formation, prevent retinal pigment epithelium (RPE) cell death, and suppress abnormal blood vessel growth, thereby preserving visual function.
Q: What are the primary considerations when developing a therapeutic agent that targets a specific complement factor?
A: Key considerations include ensuring high specificity for the target factor to avoid off-target effects, optimizing potency for effective pathway modulation, and designing for appropriate pharmacokinetic and pharmacodynamic properties. Balancing therapeutic efficacy with maintaining essential complement functions for host defense is also crucial.
Q: Can complement-targeted therapies be combined with existing treatments for AMD?
A: The potential for combination therapies is an active area of research. Integrating complement modulation with existing anti-VEGF treatments for wet AMD or other neuroprotective strategies for dry AMD could offer synergistic benefits, addressing multiple pathogenic pathways and potentially leading to more comprehensive therapeutic outcomes.
Q: How do complement-targeted approaches compare to other therapeutic strategies currently being explored for AMD?
A: Complement-targeted approaches offer a distinct advantage by addressing a fundamental inflammatory driver of AMD, which is often not fully addressed by other strategies like anti-VEGF therapies (primarily for wet AMD) or neuroprotective agents. While other strategies focus on downstream effects or specific cell types, complement modulation aims at the root cause of the disease's chronic progression.
Creative Biolabs is dedicated to advancing the understanding and therapeutic application of the complement system in AMD. Our comprehensive services, from recombinant protein supply and antibody development to advanced screening and preclinical studies, are designed to accelerate your research and bring innovative AMD treatments closer to patients.
Featured Services
Feature Products
For Research Use Only.
Related Sections: