Autoimmune Diseases Types Complement Regulatory Proteins Overview Related Products Hot Services Resources Q&A
Complement-Associated Autoimmune Diseases
Autoimmune disease treatments mainly aim to block complement activation and its receptors or the membrane attack complex. Preliminary clinical trials and preclinical studies show that adjusting the complement system could provide beneficial therapeutic outcomes for autoimmune diseases.
Systemic lupus erythematosus (SLE) presents as a serious autoimmune disease with symptoms that include fever, rash, glomerulonephritis, and hemolytic anemia. The development of SLE shows frequent connections to the deficiencies of complement components C1q, C1r, and C1s, while deficiencies in C2 and C4 components also contribute to the disease's progression. Patients with SLE experience complement system activity that leads to organ damage and autoimmune progression in B and T cell populations.
Hashimoto's disease describes an autoimmune disorder that leads to the progressive breakdown of the thyroid gland. Scientists believe that both genetic influences and environmental conditions work together to cause this disease's development. Thyroid peroxidase antibodies (TPOAb) trigger thyroid follicular cell cytolysis after interacting with the complement system that participates in this process.
Systemic sclerosis (SSc) represents a connective tissue disease that manifests with skin and organ fibrosis, which results in reduced proximal extremity movement. Patients suffering from SSc show higher levels of complement components C3d, C3d/C3, C4d, and C4d/C4 than healthy individuals.
Rheumatoid arthritis represents a primary autoimmune illness in humans that involves persistent synovial inflammation and results in the deterioration of cartilage and bone structures. Research demonstrates the essential function of complement activation in RA development with specific involvement of C3, C5aR, CR2, and MAC components.
Complement Regulatory Proteins
Autoimmune diseases that involve the complement system emerge and progress through a series of complex interrelated molecular activities. The innate immune system mistakenly identifies self-antigens, activating complement pathways through classical, lectin, or alternative means. Targeted therapeutic interventions require comprehensive knowledge of intricate molecular mechanisms to effectively modulate specific points within the complement cascade.
Table 1 Regulatory complement proteins in autoimmune disease.
|
Molecular
|
Function
|
|
C1q
|
Initiates the classical complement pathway upon binding to immune complexes formed by autoantibodies and self-antigens.
|
|
MBL/Ficolins
|
Activate the lectin pathway by binding to altered self-structures on target cells.
|
|
C3
|
A central component of all three complement pathways. Its cleavage into C3a and C3b is a major amplification step.
|
|
C3a
|
Anaphylatoxin that recruits and activates immune cells, promoting inflammation.
|
|
C3b
|
Acts as an opsonin, tagging pathogens and immune complexes for phagocytosis. Also, a component of C5 convertase.
|
|
C5
|
Its cleavage by C5 convertase generates C5a and initiates the assembly of the membrane attack complex (MAC).
|
|
C5a
|
A potent anaphylatoxin that recruits and activates immune cells, induces the release of inflammatory cytokines and chemokines, and contributes to tissue inflammation.
|
|
MAC (C5b-9)
|
A pore-forming complex that can directly lyse target cells by disrupting their membrane integrity.
|
|
CD55/CD59
|
Complement regulatory proteins present on host cell surfaces protect them from uncontrolled complement activation, particularly the alternative pathway and MAC formation. Their absence or dysfunction in self-cells can contribute to an autoimmune attack.
|
Overview of Autoimmune Disease
Historically, scientists have seen the complement system as an essential defense mechanism that identifies and removes alien organisms like bacteria and viruses through direct cellular destruction or by triggering phagocytosis as part of innate immune defense activities. Recent research has broadened our knowledge of the complement system by demonstrating its multifaceted roles in starting immune responses and controlling both innate and adaptive immune functions. Through its role in monitoring healthy cells as well as apoptotic and necrotic cells, the complement system demonstrates its essential function in preserving homeostasis.
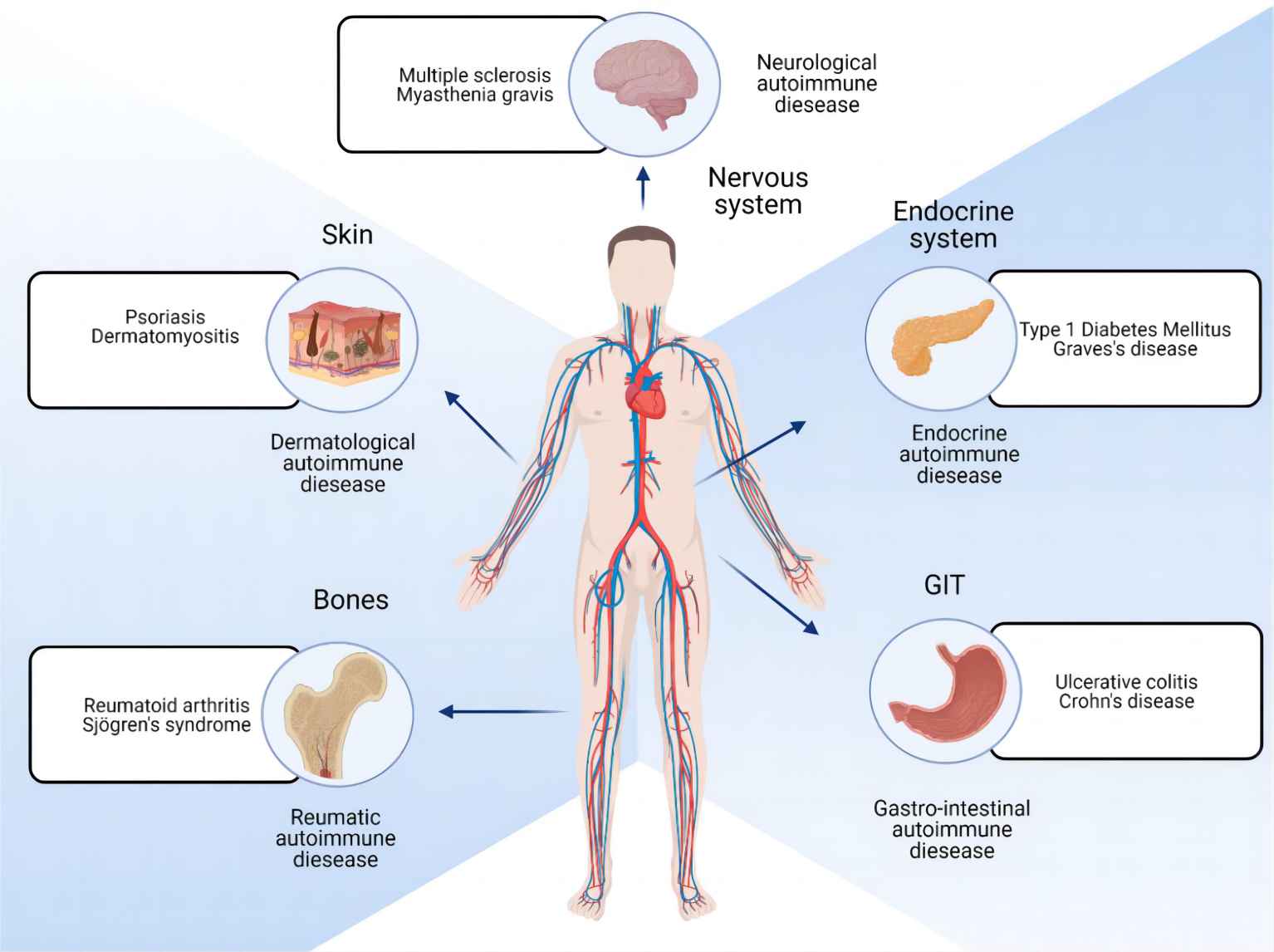 Fig. 1 Illustration of autoimmune disease. 1, 2
Fig. 1 Illustration of autoimmune disease. 1, 2
The complement network includes various zymogens and receptors together with regulatory elements that operate under strict regulation to avoid activation imbalances. Any disturbance of this sensitive equilibrium results in widespread inflammation of self-tissue. Multiple autoimmune diseases, such as SLE, vasculitides, Sjögren's syndrome, antiphospholipid syndrome, systemic sclerosis, dermatomyositis, and rheumatoid arthritis, involve dysregulation of the complement system in their pathogenesis and clinical presentations.
Pathophysiology of Autoimmune Diseases
The immune system usually recognizes the difference between foreign invaders and the body's own cells during normal conditions. In autoimmune diseases, the body's immune system mistakenly targets its healthy cells and tissues for destruction. Several pathogenic factors contribute to autoimmune diseases:
-
Emergence of Autoantigens: This process involves both the exposure of hidden antigens and changes made to existing autoantigens.
-
Abnormal Immune Regulation: Th1 and Th2 T helper cells can become dysfunctional under certain conditions.
-
Presence of Cross-Reacting Antigens.
-
Genetic and Environmental Factors.
Related Hot Products
Our extensive complement platform delivers a wide array of complement-associated products efficiently and economically. Should you have interest, please do not hesitate to reach out for further information.
Table 2 Featured products.
Related Hot Services
Table 3 Complement test services for Autoimmune disease-related complement studies.
Therapeutic antibodies, inhibitors, and soluble complement regulators, along with specialized services for complement-related autoimmune conditions, are offered by Creative Biolabs. Our all-inclusive complement platform delivers numerous complement-related products quickly and economically. Contact our team, and we will provide additional information upon request if you show interest.
Resources
References
-
Glover, Katie, Deepakkumar Mishra, and Thakur Raghu Raj Singh. "Epidemiology of ocular manifestations in autoimmune disease." Frontiers in Immunology 12 (2021): 744396.
-
Under the Open Access license CC BY 4.0, without modification.
For Research Use Only.
Related Sections:

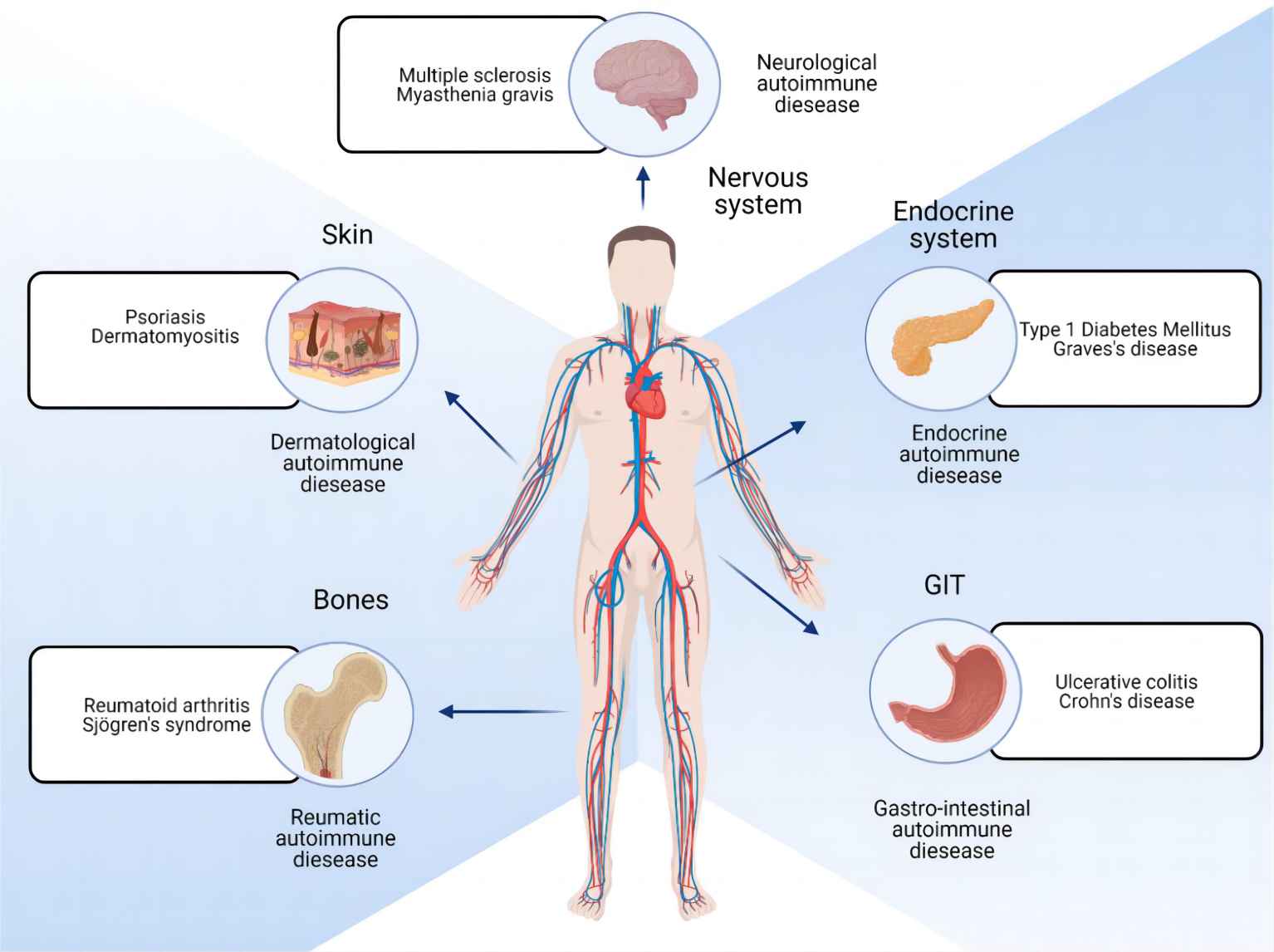 Fig. 1 Illustration of autoimmune disease. 1, 2
Fig. 1 Illustration of autoimmune disease. 1, 2