Oncolytic Viruses in Melanoma Treatment
Introduction of Melanoma
Melanoma is the least common form of skin cancer, yet associated with the highest mortality rate. Early stages of melanoma are highly curable, with a 5-year survival rate of 98%, but once metastases to other organs occur, the survival rate decreases to 15% to 20%. If diagnosed early, melanoma and surrounding normal tissue may be removed surgically, but if there is spread to lymph nodes or other organs, the options for treatment may include systemic therapy, palliative surgery/radiation, or enrollment into a clinical trial.
Several drugs for melanoma, including a cytotoxic T-lymphocyte antigen-4 inhibitor (ipilimumab), BRAF targeted agents (dabrafenib, vemurafenib), MEK inhibitors (cobimetinib, trametinib), and programmed death-1 inhibitors (nivolumab, pembrolizumab), have been approved by Food and Drug Administration (FDA). With these approval drugs, improvements in overall survival for melanoma have been reported. However, not all patients will be candidates for receiving these newer systemic agents, and after initial treatment, the melanoma may recur. Immunotherapies have transformed the landscape of melanoma treatment with exponential progress occurring in the past decade. The use of engineered oncolytic viruses has followed in that pattern and continue to evolve as additional options.
Oncolytic Viruses for the Treatment of Melanoma
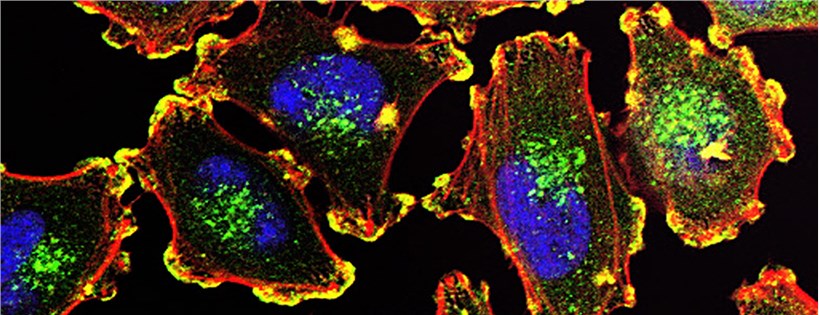
Oncolytic viruses for treating various cancers have been investigated over the past several years, and they are being evaluated as immunotherapies for a variety of advanced malignancies. These viruses selectively replicate within and lyse cancer cells without harming normal cells. Talimogene laherparepvec (T-VEC or OncoVEXGM-CSF), is the first oncolytic virus FDA approved, while there are many ongoing studies regarding other oncolytic viruses for the treatment of melanomas.
- T-VEC
- Coxsackieviruses
- HF10
- Adenovirus: telomelysin (OBP-301)
- Reovirus: Reolysin®
- Echovirus
- Newcastle Disease Virus
T-VEC is a first-in-class recombinant oncolytic virus developed from a clinical isolate of herpes simplex virus (HSV) type 1. It represents a potential treatment for patients with unresectable or metastatic melanoma, particularly in those with stage IIIB, IIIC, or IV melanoma. T-VEC has been used for the treatment of subcutaneous, unresectable cutaneous and nodal lesions in patients with melanoma recurrent after the initial surgery. T-VEC paves the way with improved outcomes for unresectable, stage IIIB-IV melanoma as a monotherapy, and has demonstrated superior results in combination with systemic checkpoint inhibitors.
Coxsackieviruses have shown potential as oncolytic treatments for melanoma. Coxsackieviruses interact with intercellular adhesion molecule-1 and decay-accelerating factor receptors, which are both overexpressed in melanoma. Cavatak® is a bio-selected and immunotherapeutic strain of coxsackievirus A21, which binds to intercellular adhesion molecule-1, the cell surface protein overexpressed on cancer cells. The safety and tolerability of combination coxsackievirus A21 injection and pembrolizumab therapy were assessed in the intra-tumoral coxsackievirus A21 and systemic pembrolizumab in advanced melanoma patients' phase 1b clinical trial. The results indicated that no dose-limiting toxicities occurred and the combination therapy was well tolerated.
HF10 is a non-engineered, non-neuroinvasive HSV-1 virus with naturally occurring deletions and insertions that decrease the virulent potential in nontumor cells while allowing for active proliferation in tumor cells. HF10 has overexpression of UL53, a gamma accessory gene that encodes glycoprotein gK which regulates HSV egression from infected cells, while HF10 also has loss of UL56, a gamma accessory gene involved in pathogenicity and latency of HSV-1, leading to the low neuroinvasive potential of the virus. A phase II trial assessed the use of intra-tumoral HF10 in stage IIIB to IV melanoma. No dose-limiting toxicities were observed. Of the 46 patients enrolled, 3 had grade 3 or higher adverse effects, including lymphedema, embolism, diarrhea, hypoglycemia, and groin pain. The best overall response rate at 24 weeks was 41%, the disease stability rate was 68%, median progression-free survival was 19 months, and overall survival was 21.8 months. Another phase II clinical trial of neoadjuvant intra-tumoral HF10 in combination with systemic nivolumab for stage IIIB-IVM1a melanoma is currently ongoing.
OBP-301 is an engineered oncolytic adenovirus with the addition of a human telomerase reverse transcriptase gene promoter. The promoter was linked to an internal ribosomal entry site that allows for selective infection and replication in tumor cells expressing telomerase. A phase I study of OBP-301 injection in various advanced solid tumors showed good tolerability with no grade 3 or 4 adverse events. Several clinical studies are ongoing, including a phase IIa trial for unresectable stage III and IV melanoma and a phase I trial of combination therapy OBP-301 with systemic pembrolizumab in advanced solid tumors.
A double-stranded RNA virus in the Reoviridae family, reovirus is nonpathogenic in humans due to inactivation in cells with functional Ras-pathway signaling. There are Ras-activating mutations in approximately 2/3 of all tumors and this virus uses this pathway for its own replication until cell lysis occurs. A phase I study demonstrated the safety of IV administration of pelareorep, a live reovirus type 3 Dearing strain. However, the phase II trial showed no objective response when given intravenously. A phase II trial of IV administration of pelareorep combined with paclitaxel/carboplatin showed an overall response rate of 21% with a 1-year overall survival of 43%. This study showed a benefit of combination therapy compared to paclitaxel/carboplatin alone.
A native, single-stranded RNA ECHO-7 virus, Rigvir® targets CD55/DAF-3, a GPI-anchored protein on cancer cells, and elicits T cell-mediated antitumor responses. A retrospective study of 79 patients with stage IA to IIC melanoma showed that patients treated with Rigvir had a 4.39- to 6.57-fold lower mortality than those who were under observation without treatment, suggesting that Rigvir® may be a useful adjuvant therapy for early-stage melanoma. Rigvir® is currently approved in Latvia and Georgia for oncolytic therapy, but there is limited evidence currently to support its efficacy in treatment.
Previous studies have shown that oncolytic Newcastle disease virus can induce immunogenic cell death in melanoma. A transcription factor STAT3 is often hyperactivated in melanoma, making it a potential target for melanoma therapy. Targeting of STAT3 by a STAT3 inhibitor suppresses oncolytic Newcastle disease virus-primed expression and release of immunogenic cell death markers in melanoma cells, which suggests Newcastle disease virus may be a potent strategy for the treatment of melanoma.
Reference
- Trager, M.H.; et al. Oncolytic viruses for the treatment of metastatic melanoma. Current Treatment Options in Oncology. 2020, 21(4):26-26.
