The complement system, also known as complement cascade, is a complex innate immune surveillance system, playing a key role in defense against pathogens and in host homeostasis. Complement was discovered many years ago as a heat-labile component of normal plasma that augments the opsonization of bacteria by antibodies and allows antibodies to kill some bacteria. This activity was said to ‘complement’ the antibacterial activity of the antibody, hence the name. Today we know that the complement both act on its own and as a ‘complement’ to the antibodies and immune cells in our host defense system. The complement system consists of a series of plasma proteins that react with one another to opsonize pathogens and include inflammatory responses that help to fight infection. A number of complement proteins are proteases that are themselves activated by proteolytic cleavage, called zymogens.
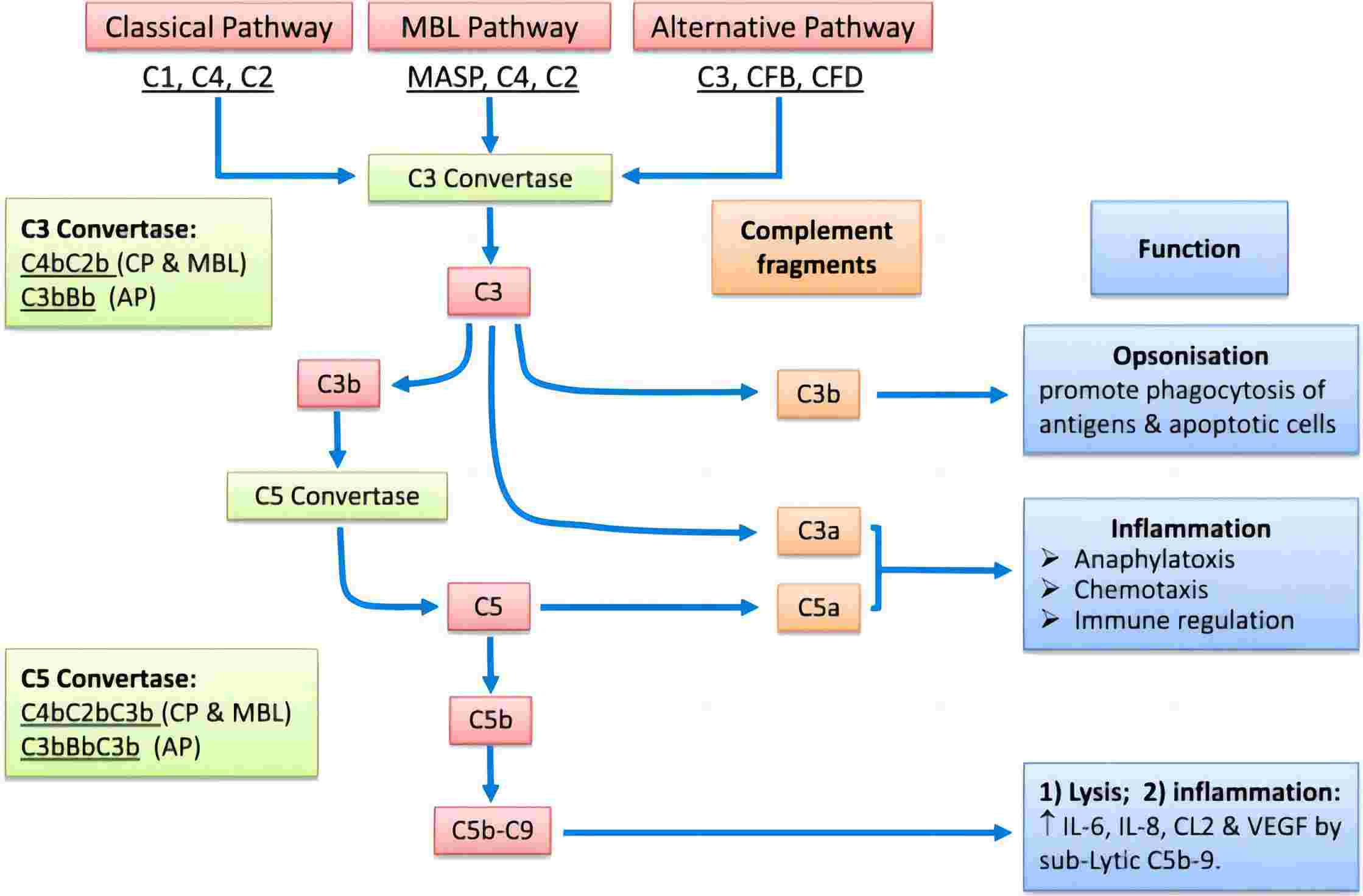
Fig. 1 Complement involvement in host defense, immune surveillance and disease processes.1,4
The complement system activates through a triggered-enzyme cascade when the innate immunity senses danger signals that disturb tissue homeostasis. In such a cascade, an active complement enzyme generated by cleavage of its zymogen precursor then cleaves its substrate, another complement zymogen, to its active enzymatic form. This, in turn, cleaves and activates the next zymogen in the complement pathway. In this way, hugely amplified responses can be produced via successive enzymatic reactions. There are three distinct pathways through which complement can be activated on pathogen surfaces: the classical pathway, lectin pathway, and alternative pathway. These pathways employ specific recognition molecules for their initiation, but they converge into a common sequence. Therefore, the complement system functions in three major ways:
-
Generation of large numbers of activated complement proteins that bind covalently to pathogens, opsonizing them for engulfment by phagocytes bearing receptors for the complement.
-
Small fragments of some complement proteins act as chemoattractants to recruit more phagocytes to the site of complement activation, and also to activate these phagocytes.
-
The terminal complement components damage certain bacteria by creating pores in the bacterial membrane through membrane attack complex (MAC).
The complement system is composed of more than 50 different molecules and cleavage products, including pattern recognition molecules, proenzymes, proteases, anaphylatoxins, opsonins, receptors, regulators, and multi-molecular complexes, etc. Each of them plays critical roles in host defense and homeostasis maintenance. To simplify and clarify complement nomenclature, and to enable rapid understanding of the intricate complement system, a list of recommended names for complement proteins has been established by the International Complement Society (ICS) and the European Complement Network (ECN) in 2014. More efforts are being made in order to improve the uniformity and simplicity of the nomenclature of this system.
Role of Complement in Different Diseases
Various mechanisms have been reported to disrupt the balance between complement activation and regulation, resulting in over-activation, damage, and disease. For example, adverse complement activation can be triggered after exposure to massive amounts of pathogen, damage-associated stimuli or foreign surfaces such as transplanted organs or biomaterials. Moreover, in many chronic disorders, mutations in the complement genes can lead to a systemic or local imbalance thereby contributing to inflammation, thrombosis, and tissue damage. In addition, deficiencies in the complement proteins can lead to ineffective removal of apoptotic cells, debris or immune complexes, thereby inducing or exacerbating autoimmune and neurodegenerative diseases. In summary, Excessive or insufficient activation will break the delicate balance between complement activation and regulation, leading a variety of disease, including:
Complement as A Therapeutic Target
Association of complement with common and devastating diseases has driven an upsurge in complement drug discovery. Efforts have been focused on different complement system components as therapeutic targets. Major targets include C3, C5, and therapeutic target C5aR1. Other potential targets include Factor D, Factor B, MASP2, C1 complex, etc. More than 20 therapeutic agents targeting distinct components and effector pathways of the complement cascade are now in clinical development for various indications. Based on the diverse mechanism of actions, the current complement therapeutics can be classified into five major categories:
-
Serine Protease Inhibitors
-
Soluble Complement Regulators
-
Therapeutic Antibodies in Complement Therapeutic
-
Complement Component Inhibitors
-
Anaphylatoxin Receptor Antagonists
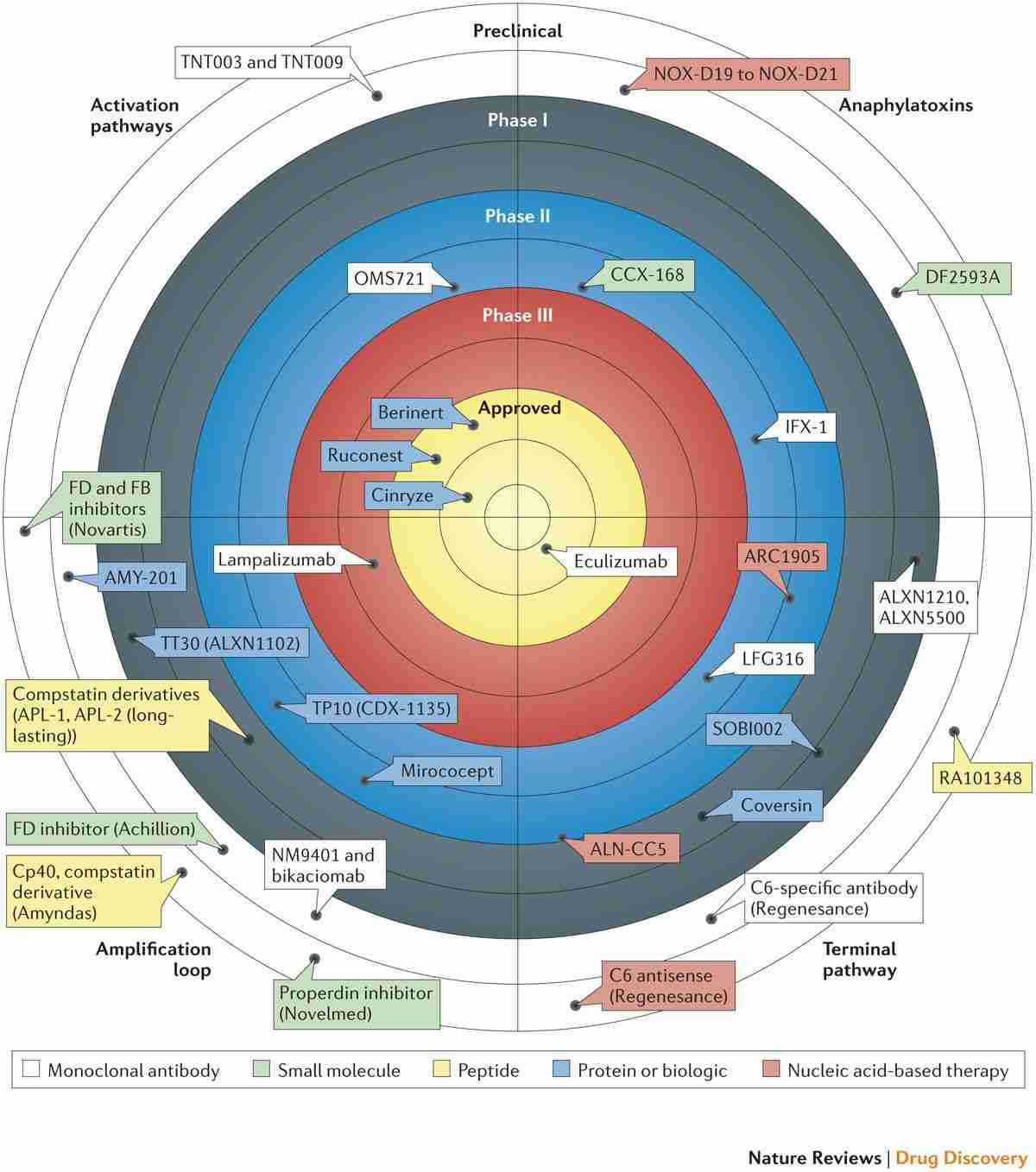
Fig. 2 Advancements in complement therapeutics for clinical application.2,4
Especially, Creative Biolabs offers complement drug discovery services targeting various complement components for different indications. Besides, we offer complement testing services, including complement function test, complement autoantibody test, and complement genetic test.
Published Data
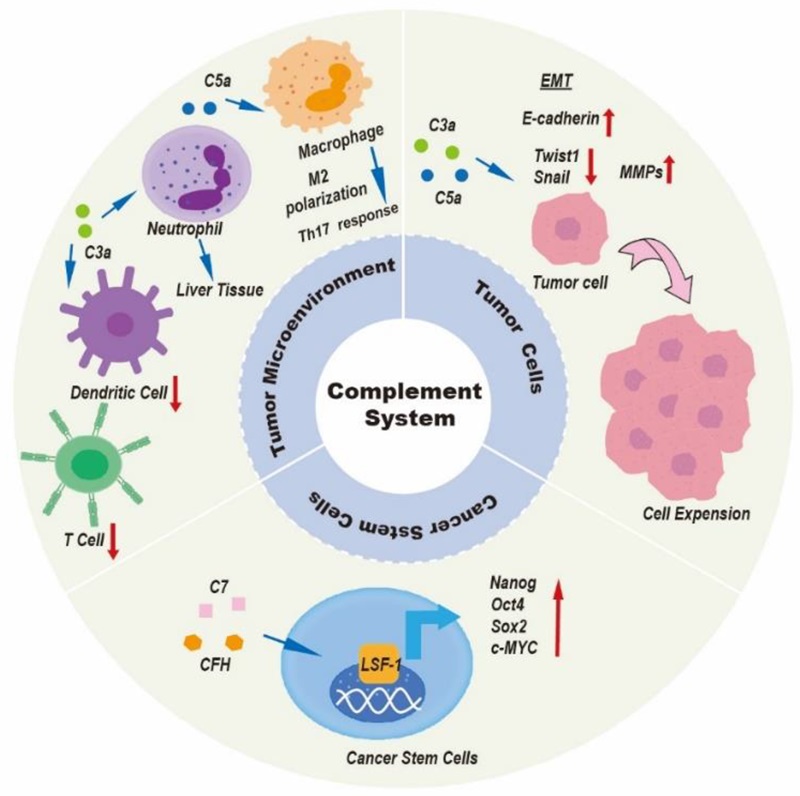 Fig.3 Overview of the complement system
Fig.3 Overview of the complement system
The complement system, an important element of the immune defense, plays a significant role in mediating both innate and adaptive immune reactions. It initiates anti-cancer effects by recognizing tumor cells as foreign entities, triggering cytotoxic effects that target these cells. However, within the context of tumor progression, the complement system serves a dual function. It engages in multiple biological processes that influence liver cancer progression through its regulatory impact on the tumor microenvironment, cancer cells, and stem cells. Specifically, the complement system can reinforce immunosuppression within tumors, aid in forming premetastatic niches, enhance invasion and proliferation of tumors, promote angiogenesis, and activate cancer stem cells, thus fostering tumor progression.
References
-
Xu, Heping, and Mei Chen. "Targeting the complement system for the management of retinal inflammatory and degenerative diseases." European journal of pharmacology 787 (2016): 94-104.
-
Meuleman, Marie-Sophie, et al. "Ex vivo test for measuring complement attack on endothelial cells: from research to bedside." Frontiers in Immunology 13 (2022): 860689.
-
Yuan, Meng, et al. "The complement system: a potential therapeutic target in liver cancer." Life 12.10 (2022): 1532.
-
Distributed under Open Access license CC BY 4.0, without modification.
Related Product
For Research Use Only.
Related Sections:

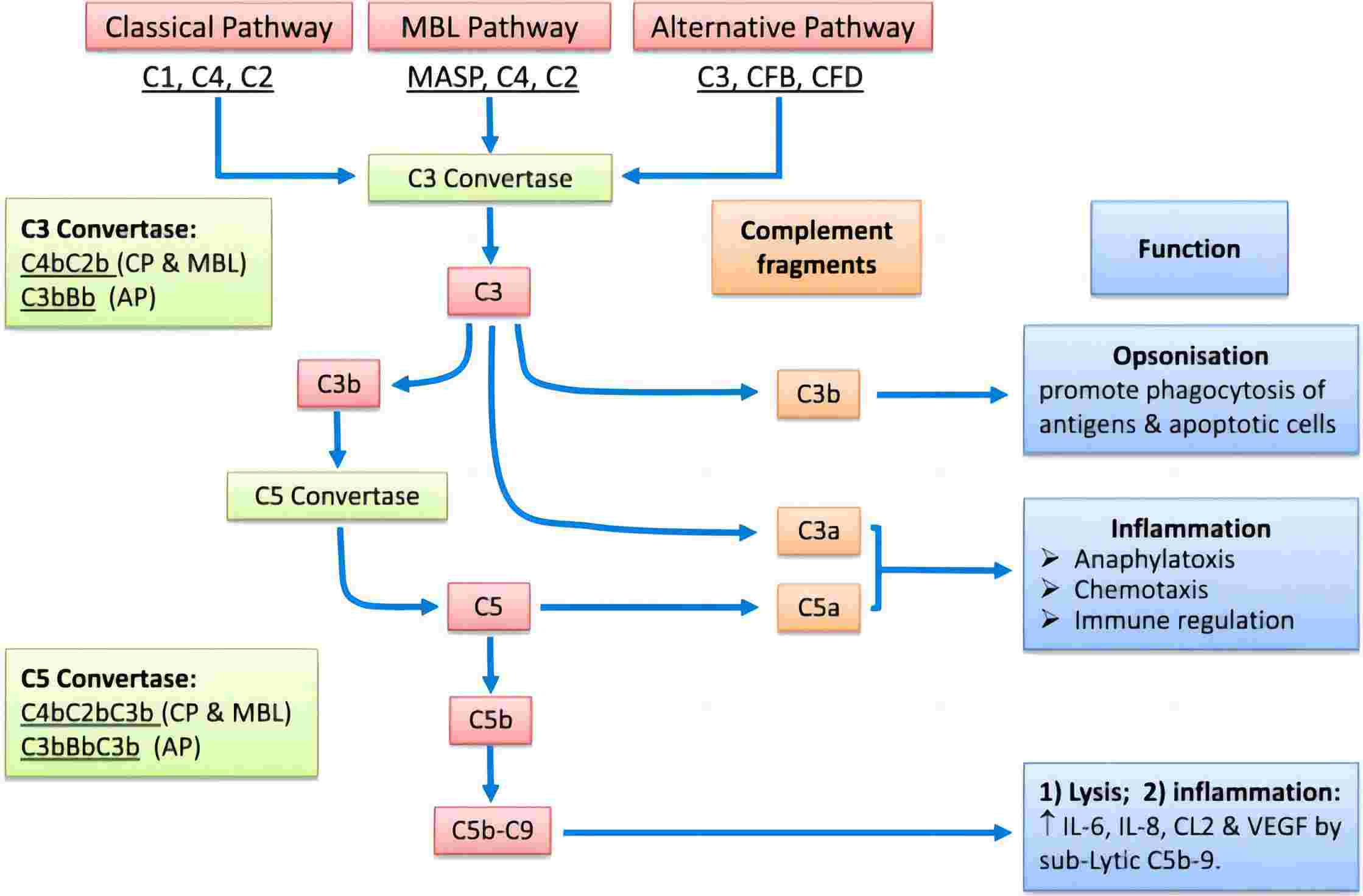
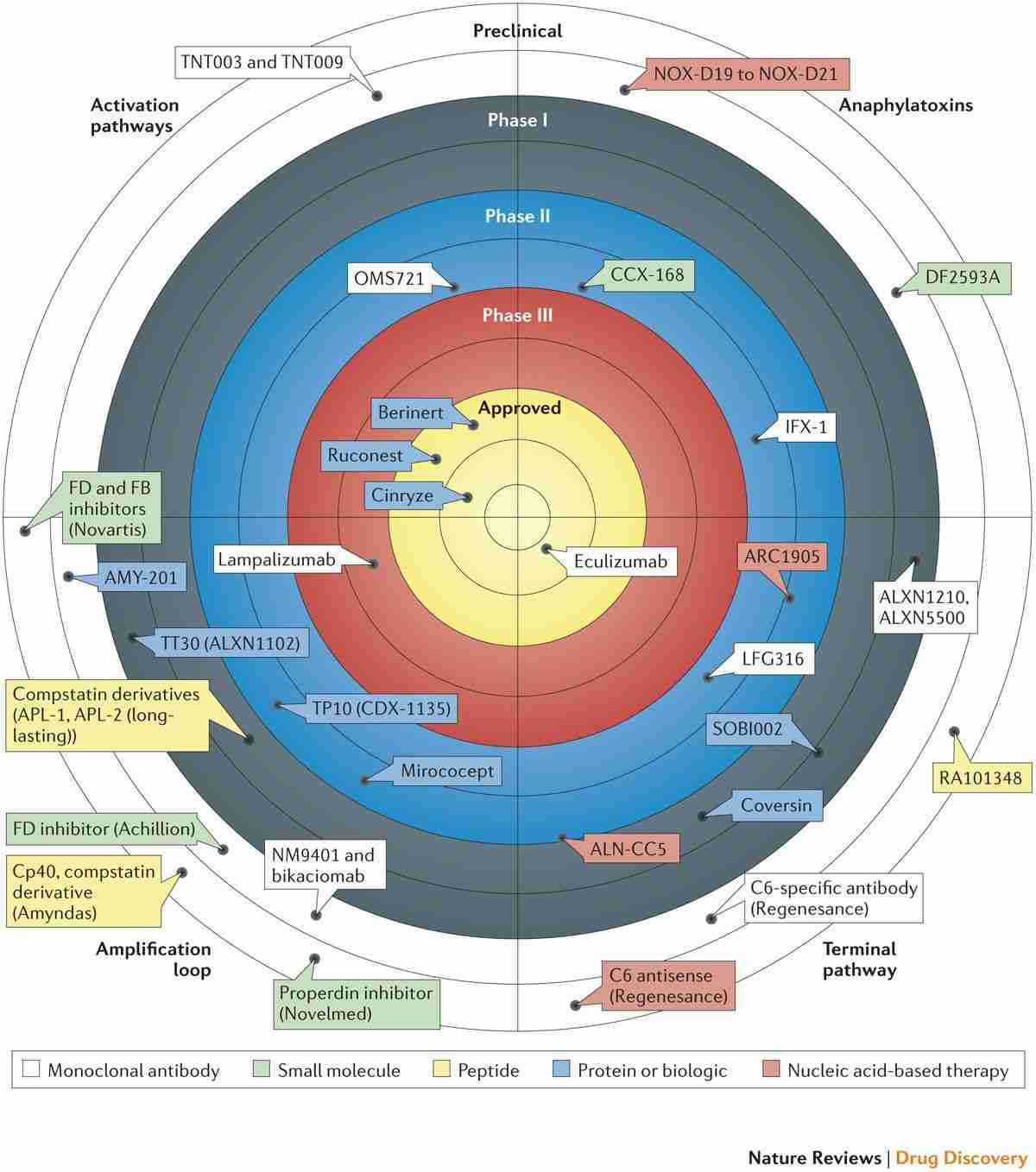
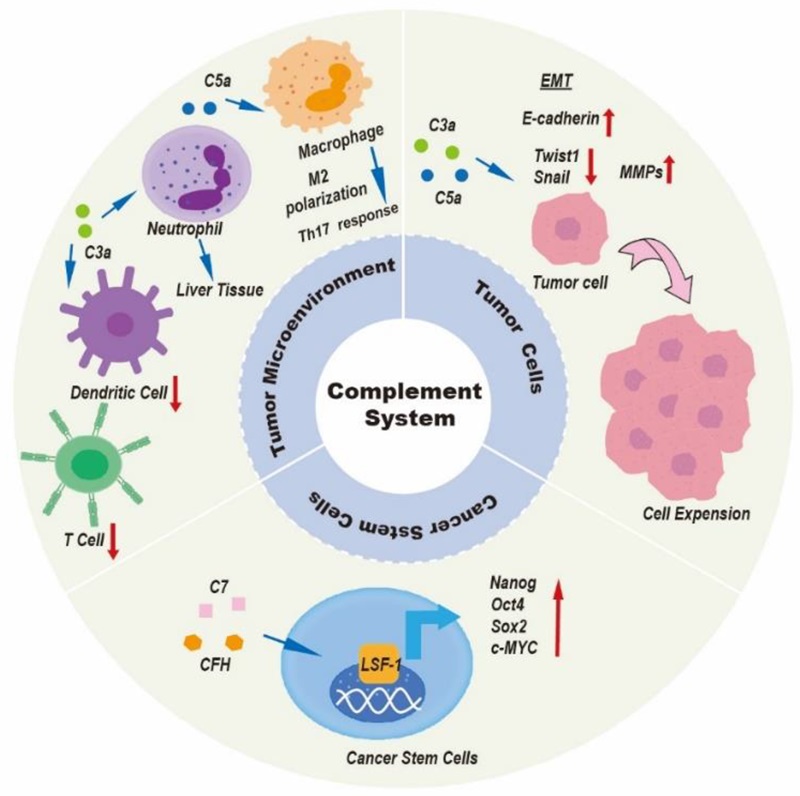 Fig.3 Overview of the complement system
Fig.3 Overview of the complement system