T cells, or T lymphocytes, come from yolk sac in embryonic stage and liver pluripotent stem cells in bone marrow. In the embryonic and neonatal stages, some pluripotent stem cells or pre-T cells in bone marrow migrate to the thymus, differentiate and mature under the induction of thymic hormones, and become T cells with immune activity.
Mature T cells are distributed through blood flow to the thymic dependent area of peripheral immune organs, and can be recycled through lymphatic vessels, peripheral blood and tissue fluid, so as to exert the functions of cellular immunity and immune regulation. The recirculation is beneficial for the T cells to extensive exposure to antigen substances entering the body, strengthen the immune response, and maintain immune memory for a long time. There are many different markers on the cell membrane of T cells, mainly surface antigens and receptors, which participant in the T cell-mediated immune responses.
Classification of T Cells
T cells are quite complex and heterogeneous subsets that are constantly renewed in the body and can exist at different developmental stages or functions at the same time, but the classification principles and naming are confused and have not yet been unified. According to the different functions of the immune response, T cells can be divided into several subsets, which are unanimously recognized as follows:
(1) Helper T cells (Th), which are also called CD4+ cells because they express cluster of differentiation (CD) 4 (CD4) on the surface. They are activated by the reaction of polypeptide antigen presented with major histocompatibility complex (MHC) class II (MHC-II). MHC-II is expressed on the surface of antigen-presenting cells (APCs). Once activated, cytokines can be secreted to regulate or assist the immune response.
(2) Suppressor T cells (Ts), which have the function of inhibiting cellular immunity and humoral immunity.
(3) Effector T cells (Te), which have the function of releasing lymphoid factor.
(4) Cytotoxic T cells (Tc), or cytotoxic T lymphocytes (CTLs), also known as CD8+ cells for expressing CD8 on the surface, can bind directly to antigens through MHC class I (MHC-I) and have the function of killing target cells.
(5) Delayed type hypersensitivity T cells (Td), which participate in type IV allergic reaction.
(6) Memory T cells (Tm), which has the effect of memory specific antigen stimulation. T cells can survive in the body for months to years, and the memory cells survived longer.
(7) Virgin or Natural T cells, which differentiate into effector and memory T cells after contact with antigens.
T Cell-mediated Immune Responses
T cells are the main components of lymphocytes. They have a variety of biological functions, such as killing target cells directly, assisting or inhibiting the production of antibodies by B cells, responding to specific antigens and mitogen, and producing cytokines. It is a brave fighter formed in the body to resist disease, infection and tumor. The immune response produced by T cells is cellular immunity, and there are two main forms of cellular immunity: one is specifically binding to target cells, destroying target cell membrane and killing target cells directly; the other is the release of lymphokines, which eventually expands and enhances the immune effect.
The initial T cells (naïve T cells) mature and migrate out of the thymus, settle in the peripheral lymphoid organs with the blood circulation and recycle in the body. When the initial T cells specifically bind to the antigen peptide-MHC (pMHC) complex on the surface of APC, the T cells are activated, proliferated and differentiated into effector T cells under the action of auxiliary factors, completing the clearance of antigen and the regulation of immune responses. In these processes, some activated T cells differentiate into memory T cells. The T cell-mediated immune responses are also called cellular immune responses, which are continuous processes and can be divided into three stages: antigen recognition by T cells, the activation, proliferation and differentiation of T cells, and the generation and effect of effector T cells.
The T cell receptors (TCRs) of the initial T cells specifically binds to the pMHC presented by APC, which is the first step of T cell specific activation. While TCR specifically recognizes the antigen peptide presented by APC, it must also recognize its own MHC molecules in the complex. This MHC restriction determines that any T cell only recognizes pMHC submitted by the same individual APC. The presentation process and mechanism of exogenous antigen and endogenous antigen are different. Exogenous antigens are presented to specific CD4+ T cells for recognition by MHC-II molecules. CD4+ T cells play different functions by producing cytokines to regulate cellular and humoral immune responses. Endogenous antigens are presented to specific CD8+ CTL for recognition through MHC-I molecules.
The complete activation of T cells depends on the action of double signals and cytokines. T cell activation is the basis of T cell proliferation and differentiation. Once APC presents pMHC-II to T cells, the TCRs specifically recognizes the antigenic peptides bound to the MHC trough, resulting in the interaction between CD3 and the cytoplasmic segment of the co-receptor (CD4 or CD8), activating the protein tyrosine kinase. The tyrosine phosphorylation in the plasmalemma immunoreceptor tyrosine-based activation motif (ITAM) of CD3 initiates the signal transduction activated, and finally causes the activation and transcription of a variety of membrane molecules and cell activation-related genes by activating transcription factors, resulting in the initial activation of T cells. This is the first signal of T cell activation (that is, antigen stimulation signal). At the same time, APC in contact with T cells is also activated to up-regulate the expression of costimulatory molecules. The interaction between many pairs of costimulatory molecules on the surface of T cells and APCs (such as CD28, CTLA-4 and CD80, CD86, PD-1 and PD-L1 and PD-L2, ICOS and ICOSL, CD40L and CD40) produces the second signal (costimulatory signal) of T cell activation, resulting in the completely activation of T cells. A series of signals in activated T cells induce the expression of a variety of cytokines and cytokine receptors. Activated APC also produces cytokines to promote the proliferation and differentiation of T cells. If there is a lack of costimulatory signal, the first signal cannot effectively activate specific T cells, but leads to T cell disability.
After being fully activated, T cells also depend on the effects of more than a thousand cytokines (IL-1, IL-2, IL-4, IL-6, IL-10, IL-12, IL-15 and IFN-γ, etc.) for further proliferation and differentiation. Among these cytokines, IL-2 is very important for T cell proliferation, and other cytokines are involved in T cell differentiation. Lack of cytokines will result in apoptosis of the activated T cells.
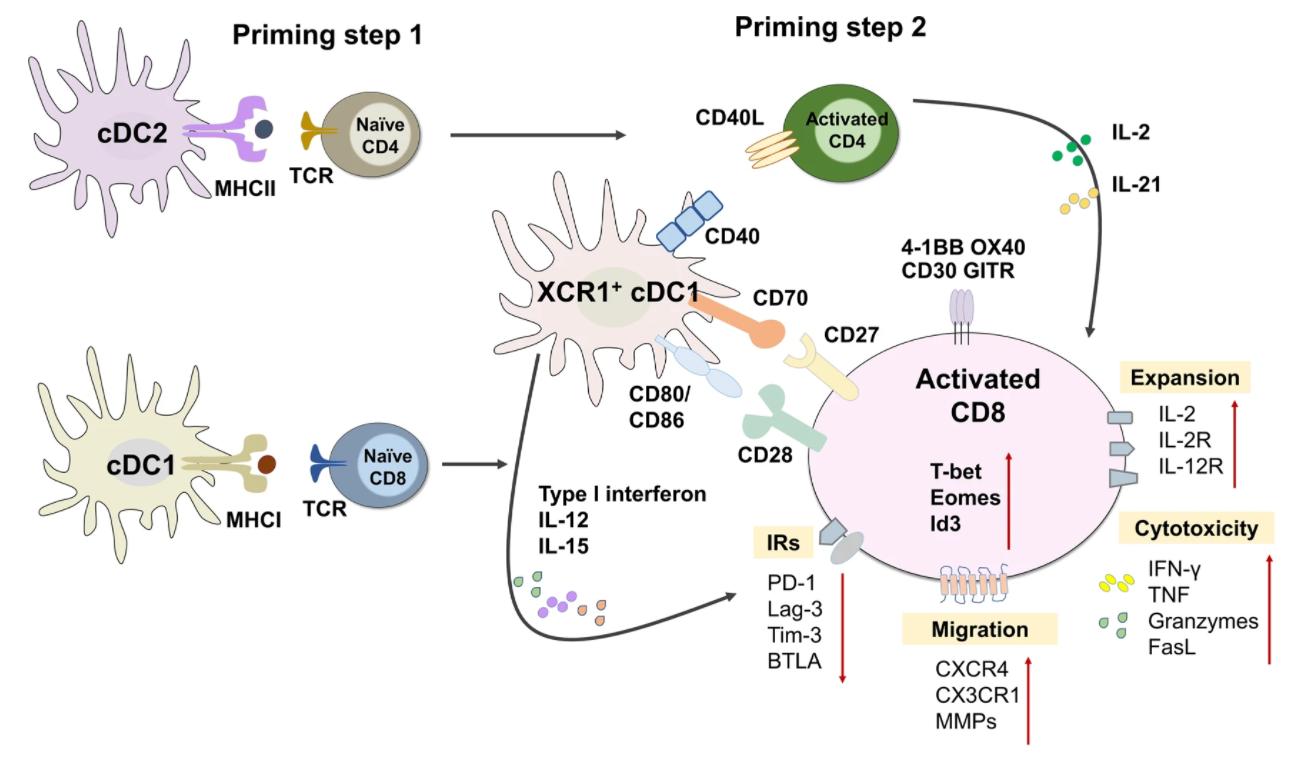 Fig.1 Cellular immunity.1
Fig.1 Cellular immunity.1
T cells cloned and expanded through mitosis further differentiate into effector T cells under the action of different cytokines.
The initial CD4+T cell (Th0) is regulated by different cytokines to differentiate into different directions in the local microenvironment, and its differentiation direction determines the type of immune response. IL-12 and IFN-γ can induce Th0 to differentiate into Th1, which mainly mediates cellular immune response. IL-4 can induce Th0 to differentiate into Th2, which mainly mediates humoral immune response. TGF-β and IL-2 can induce Th0 to differentiate into regulatory T cell (Treg), which plays an important role in maintaining autoimmune tolerance by secreting IL-10, TGF-β or direct contact with cells. TGF-β and IL-6 (mouse) or IL-1β and IL-6 (human) can induce Th0 to differentiate into Th17, which not only stimulate a variety of cells to participate in the immune defense by secreting IL-17, but also participate in the pathogenesis of autoimmune diseases. IL-21 and IL-6 could induce Th0 to differentiate into Tph, which migrates to lymphoid follicular and assist B cells in producing antibodies. Partially activated Th can also differentiate into memory cells and play an important role in the re-immune response.
There are two main ways to activate and differentiate CD8+ T cells. The first way is Th-dependent: target cells cannot effectively activate the initial CD8+ T cells, but need the assistance of APC and Th. The intracellular viral antigen and tumor antigen, as well as the exfoliated donor allogenic MHC antigen, are ingested by APC in a soluble form and bind to MHC-I molecules and MHC-II molecules to form complexes in the cells. After pMHC-II binds to TCR, Th is activated. pMHC-I binds to TCR to activate CTL precursor cells, which proliferate and differentiate into CTLs under the combined action of specific activation signal of pMHC-I and cytokines released by Th cells. The second way is that Th cells are independent: viruses with highly expressed costimulatory molecules infect dendritic cells (DCs), directly stimulating CD8+ T cells to produce IL-2 and inducing CD8+ T cells to proliferate and differentiate into CTL without the assistance of Th cells.
CTL can kill intracellular pathogens (viruses and some intracellular parasitic bacteria) efficiently and specifically to infect target cells such as cells and tumor cells without damaging normal cells. The effect process of CTL includes recognition and binding of target cells, intracellular organelle reorientation, granular exocytosis and target cell disintegration. CTL can also produce cytokines to regulate immune response. CTLs kill target cells mainly through two pathways. (1) Perforin/granzyme pathway. Perforin and granzyme are stored in cytoplasmic granules. In the presence of calcium ion, several perforins synthesize pores with an inner diameter, which makes the cytotoxicity proteins such as granzyme enter the cell rapidly. Granzyme is a kind of serine protease, which can induce apoptosis of target cells by activating apoptosis-related enzyme system. (2) Death receptor pathway. CTLs can express membrane Fas ligand (FasL) and soluble FasL (sFasL) or secrete TNF. These effector molecules can bind to Fas and TNF receptors on the surface of target cells and induce apoptosis of target cells by activating the signal transduction pathway involved by intracellular caspase.
T Cell-based Immunotherapies
Based on the significant roles of T cells in the immune system, many small-molecule drugs targeting T cells and T-cell based immunotherapies have been developed for the treatment of intractable diseases including autoimmune diseases and cancer. T cell-based immunotherapies mainly utilize the mechanisms of T cell-mediated immune responses and the effects of some other immune cells such as dendritic cells (DCs), natural killer (NK) cells, and macrophages. Currently developed T cell-based immunotherapies mainly include monoclonal antibodies targeting T cells, adoptive transfer of genetically engineered T cells, and T cell vaccine.
 Monoclonal antibody therapy is the use of monoclonal antibodies (mAb) to specifically target cells. The main objective is stimulating the patient's immune system to attack the malignant tumor cells and the prevention of tumor growth by blocking specific cell receptors. Monoclonal antibody-based treatment of cancer has been established as one of the most successful therapeutic strategies for both hematologic malignancies and solid tumors in the last 20 years.
Monoclonal antibody therapy is the use of monoclonal antibodies (mAb) to specifically target cells. The main objective is stimulating the patient's immune system to attack the malignant tumor cells and the prevention of tumor growth by blocking specific cell receptors. Monoclonal antibody-based treatment of cancer has been established as one of the most successful therapeutic strategies for both hematologic malignancies and solid tumors in the last 20 years.
 With the development of biotechnologies especially gene editing techniques, engineering of somatic cells is getting easier and more efficient. Owing to the unique immune functions of T cells, adoptive transfer of autologous or allogenic T cells gene-engineered with antigen-specific receptors, whether it be chimeric antigen receptors (CARs) or T cell receptors (TCRs), has proven its feasibility and therapeutic potential in the treatment of tumors according to the data from clinical applications.
With the development of biotechnologies especially gene editing techniques, engineering of somatic cells is getting easier and more efficient. Owing to the unique immune functions of T cells, adoptive transfer of autologous or allogenic T cells gene-engineered with antigen-specific receptors, whether it be chimeric antigen receptors (CARs) or T cell receptors (TCRs), has proven its feasibility and therapeutic potential in the treatment of tumors according to the data from clinical applications.
 T cell-inducing vaccine is a type of vaccine that stimulates the immune system to produce T cells, which play a crucial role in fighting infections and cancer. Unlike traditional vaccines, which mainly stimulate the production of antibodies, T cell-inducing vaccines target T cells, which can recognize and kill infected cells or cancer cells directly. These vaccines are especially beneficial in preventing and treating diseases that are caused by viruses and tumors that can evade the immune system's recognition. Recent advances in vaccine technology have shown promising results in developing T cell-inducing vaccines, which have the potential to revolutionize the field of immunotherapy and improve global health outcomes.
T cell-inducing vaccine is a type of vaccine that stimulates the immune system to produce T cells, which play a crucial role in fighting infections and cancer. Unlike traditional vaccines, which mainly stimulate the production of antibodies, T cell-inducing vaccines target T cells, which can recognize and kill infected cells or cancer cells directly. These vaccines are especially beneficial in preventing and treating diseases that are caused by viruses and tumors that can evade the immune system's recognition. Recent advances in vaccine technology have shown promising results in developing T cell-inducing vaccines, which have the potential to revolutionize the field of immunotherapy and improve global health outcomes.
Reference
For any technical issues or product/service related questions, please leave your information below. Our team will contact you soon.
All products and services are For Research Use Only and CANNOT be used in the treatment or diagnosis of disease.
 NEWSLETTER
NEWSLETTER
The latest newsletter to introduce the latest breaking information, our site updates, field and other scientific news, important events, and insights from industry leaders
LEARN MORE NEWSLETTER NEW SOLUTION
NEW SOLUTION
CellRapeutics™ In Vivo Cell Engineering: One-stop in vivo T/B/NK cell and macrophage engineering services covering vectors construction to function verification.
LEARN MORE SOLUTION NOVEL TECHNOLOGY
NOVEL TECHNOLOGY
Silence™ CAR-T Cell: A novel platform to enhance CAR-T cell immunotherapy by combining RNAi technology to suppress genes that may impede CAR functionality.
LEARN MORE NOVEL TECHNOLOGY NEW SOLUTION
NEW SOLUTION
Canine CAR-T Therapy Development: From early target discovery, CAR design and construction, cell culture, and transfection, to in vitro and in vivo function validation.
LEARN MORE SOLUTION