Lipid-Based Drug Delivery Systems in Tuberculosis Treatment
Background Biological Barriers Key Delivery Systems Creative Biolabs' Solutions Why Choose Us? Workflow Published Data Related Services Resources
Tuberculosis (TB) continues to be a formidable global health challenge, demanding urgent innovation in treatment and diagnosis. The efficacy of current anti-TB drugs is often compromised by issues such as short drug half-life, rapid drug degradation, low drug concentration at the site of infection, and significant off-target effects. Creative Biolabs expertise in lipid-based drug delivery systems helps you accelerate drug discovery and enhance therapeutic outcomes through innovative nano-encapsulation technologies and targeted delivery strategies.
Background of Tuberculosis
Tuberculosis (TB), an infectious disease caused by the bacterium Mycobacterium tuberculosis, remains a leading cause of morbidity and mortality worldwide, second only to COVID-19. As an airborne disease, it primarily affects the lungs (pulmonary TB) but can also impact other parts of the body (extrapulmonary TB), including the brain, spine, and kidneys. Common complications include lung damage, spinal pain, kidney impairment, and cardiac tamponade.
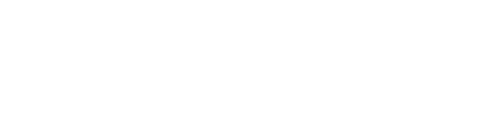
The pathophysiology of tuberculosis begins when an individual inhales airborne droplets containing M. tuberculosis. These bacilli typically reach the alveoli of the lungs, where they are engulfed by alveolar macrophages. Inside these macrophages, the bacteria can survive and multiply, resisting the host's immune defenses. In most cases, the immune system contains the infection by forming granulomas – compact, organized aggregates of immune cells (macrophages, lymphocytes, and fibroblasts) that wall off the bacteria. This leads to latent TB infection, where the bacteria remain dormant but viable. However, if the host's immune system weakens, these latent bacilli can reactivate, leading to active TB disease.
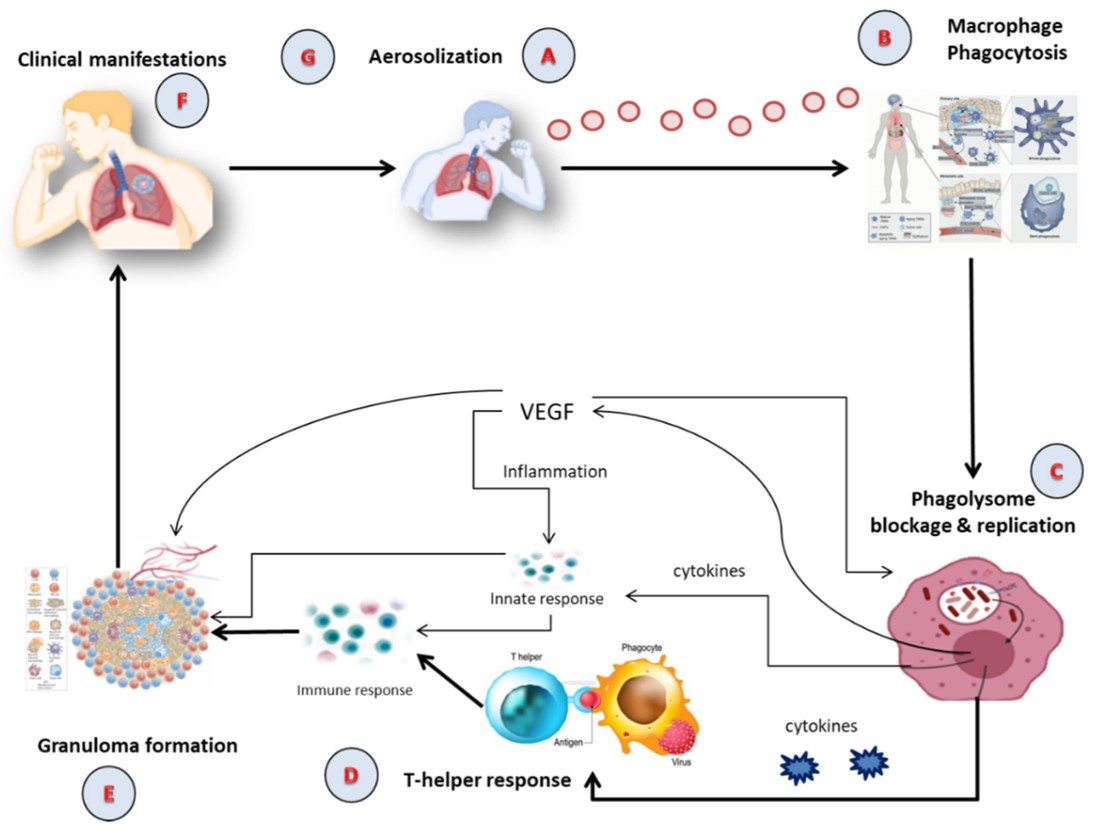 Fig. 1 The pathophysiology of active TB.1,3
Fig. 1 The pathophysiology of active TB.1,3
Biological Barriers to Effective Delivery of Anti-TB Drugs
The unique pathogenesis of TB presents formidable biological obstacles that conventional drugs struggle to overcome, particularly in the context of pulmonary administration. These barriers contribute significantly to the challenges of achieving effective drug concentrations at the site of infection and include:
-
Mucus Layer: The lung's mucus layer, rich in mucins, forms a physical and electrostatic barrier. Its small pore size (~340 nm) and negative charge hinder nanoparticles penetration, leading to retention via bio-nano interactions.
-
Pulmonary Surfactant (PS): PS, a lipoprotein complex, can promote drug adhesion and agglutination by immune cells (such as mucosal cilia, macrophages, and monocytes). It may also contribute to the clearance of therapeutic agents from the lungs, reducing their availability.
-
Immune Cell Clearance: Respiratory immune cells, like macrophages and dendritic cells, actively internalize inhaled drugs. This size- and opsonin-dependent phagocytosis, particularly by abundant macrophages, is a major mechanism for drug clearance from the lungs.
-
Metabolic Enzymes: Lung epithelial cells contain enzymes (e.g., trypsin, antitrypsin, proteases) that metabolize and break down therapeutic drugs. This enzymatic degradation reduces drug concentration and efficacy at the target site.
-
Biofilm Formation: In chronic infections, bacterial biofilms form structured communities encased in an extracellular matrix. This physical barrier significantly impedes the penetration of antimicrobial agents, making treatment of biofilm-associated TB challenging.
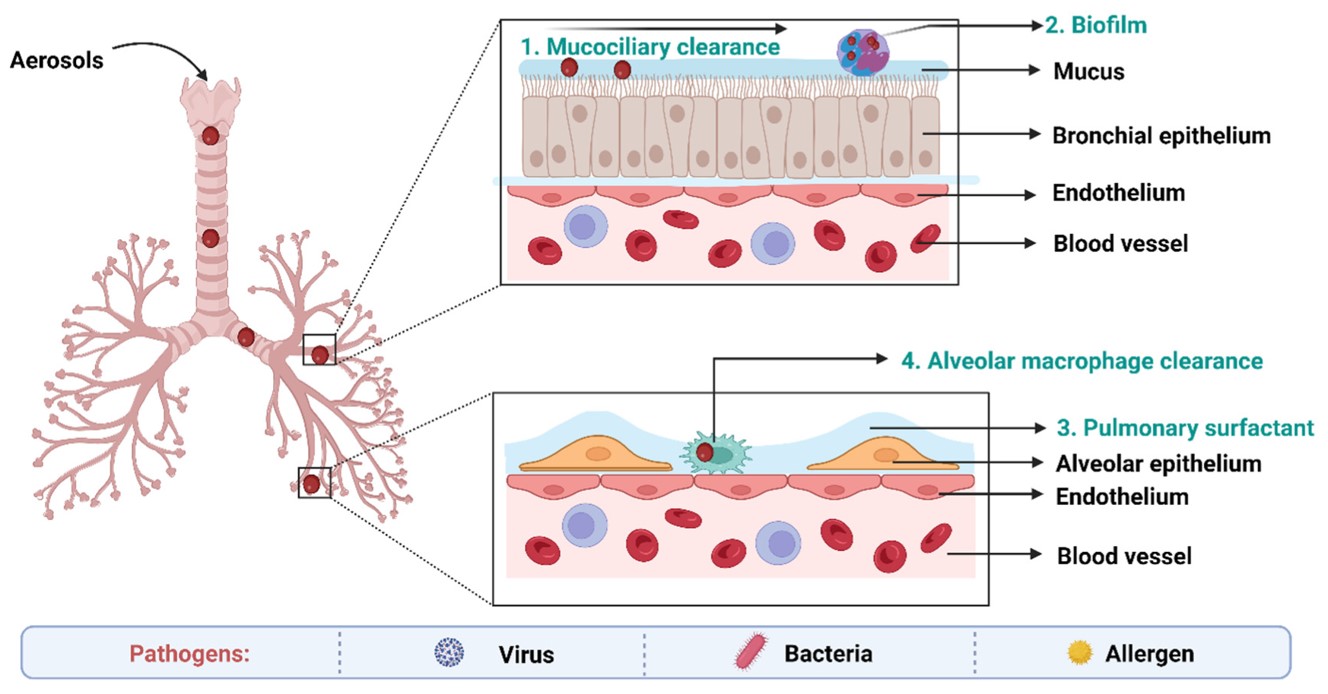 Fig. 2 Biological barriers in targeted drug delivery to lungs in TB.1,3
Fig. 2 Biological barriers in targeted drug delivery to lungs in TB.1,3
These inherent challenges underscore the urgent need for advanced drug delivery strategies that can overcome biological barriers, enhance drug efficacy, reduce toxicity, and simplify treatment regimens.
Key Lipid-Based Drug Delivery Systems for Anti-TB Drugs
At Creative Biolabs, we recognize that overcoming these challenges requires innovative solutions. Lipid-based drug delivery systems represent a paradigm shift, offering a sophisticated approach to enhance the therapeutic index of anti-TB drugs. By encapsulating drugs within lipidic carriers, we can achieve:
-
Enhanced Bioavailability: Improved solubility and absorption of poorly soluble drugs.
-
Reduced Systemic Toxicity: Lower drug exposure to healthy tissues, minimizing adverse effects.
-
Targeted Delivery: Preferential accumulation in macrophages and granulomas, where the bacteria reside.
-
Sustained Release: Prolonged drug action, potentially reducing dosing frequency and improving patient compliance.
-
Overcoming Drug Resistance: Bypassing efflux pumps and improving intracellular drug concentrations.
-
Improved Stability: Protecting sensitive drugs from degradation in the physiological environment.
Liposomes
Liposomes are spherical lipid vesicles encapsulating drugs. They enhance delivery to macrophages, crucial for targeting intracellular M. tuberculosis, improving efficacy and reducing systemic toxicity of anti-TB drugs like rifampicin and isoniazid.
Nanoemulsions
Nanoemulsions are thermodynamically stable isotropic mixtures of oil, water, and surfactant. They significantly enhance the solubility and bioavailability of lipophilic anti-TB drugs, enabling rapid absorption and improved penetration into infected tissues, ideal for pulmonary delivery.
Solid Lipid Nanoparticles (SLNs)
SLNs are colloidal carriers made from solid lipids, offering high drug loading capacity and excellent stability. They provide sustained release and improve oral bioavailability of poorly soluble anti-TB drugs, potentially reducing dosing frequency.
Nanostructured Lipid Carriers (NLCs)
NLCs are advanced versions of SLNs, incorporating both solid and liquid lipids. NLCs are particularly effective in delivering drugs like linezolid and ethambutol, improving their therapeutic efficacy and reducing toxicity.
How Creative Biolabs' Lipid-Based Drug Delivery Systems Can Assist Your Project
Various anti-TB drugs, both first-line and second-line, can be effectively loaded into lipid-based drug delivery systems to enhance their therapeutic profiles. The choice of lipid-based drug delivery systems depends on the drug's physiochemical properties and the desired delivery outcome.
Beyond drug therapy, lipid-based drug delivery systems hold immense promise for the development of next-generation TB vaccines. These systems can effectively encapsulate and deliver vaccine antigens and adjuvants, enhancing their immunogenicity and directing immune responses towards protective pathways.
-
Improve Antigen Presentation: Facilitate efficient uptake and presentation of TB antigens by antigen-presenting cells, such as dendritic cells and macrophages.
-
Potentiate Immune Responses: Act as effective adjuvants, stimulating robust and long-lasting cell-mediated and humoral immune responses crucial for TB protection.
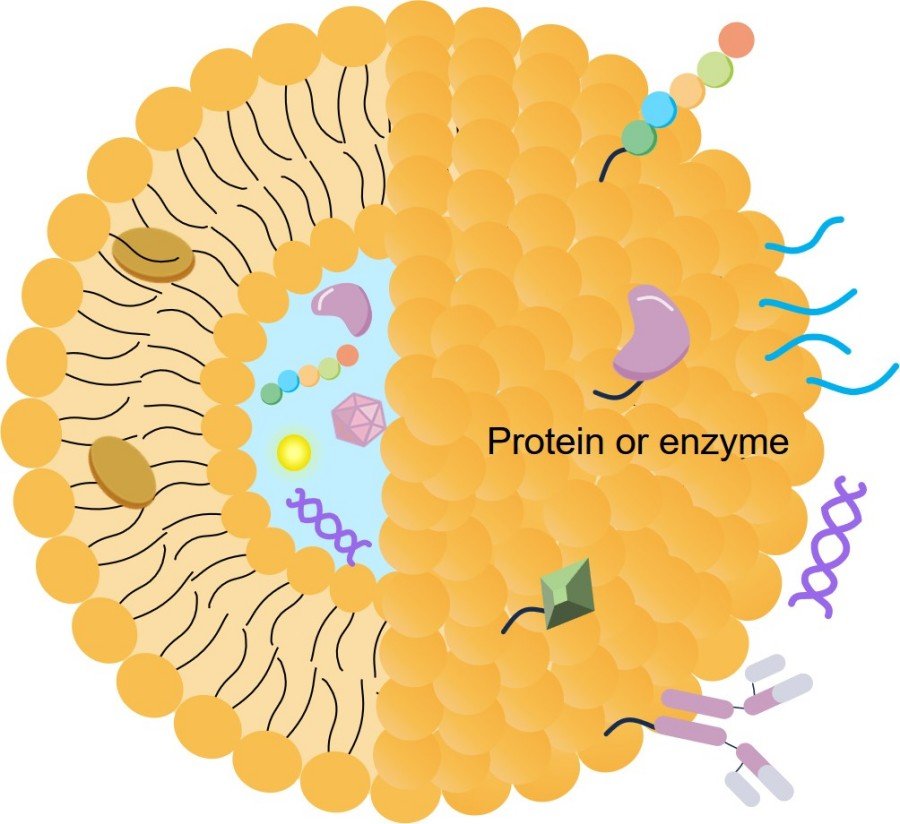
Creative Biolabs further enhances the efficacy of lipid-based drug delivery systems for anti-TB drugs by employing advanced ligand conjugate strategies. By attaching specific targeting ligands to the surface of nanoparticles, we can achieve highly precise delivery, enabling these systems to bypass biological barriers and specifically target infected alveolar macrophages or granulomas. This approach significantly improves the therapeutic index and reduces off-target effects.
 Fig. 3 Drug targeting employing conjugation of ligands with drug-loaded nanocarriers in TB.1,3
Fig. 3 Drug targeting employing conjugation of ligands with drug-loaded nanocarriers in TB.1,3
Discover How We Can Help - Request a Consultation
Why Choose Us?
At Creative Biolabs, our deep expertise in lipid-based drug delivery systems is tailored to meet the evolving research and development needs of our clients in the fight against TB. We offer comprehensive solutions that translate cutting-edge science into tangible results.
-
Formulation Development: Design and optimization of novel delivery systems formulations (liposomes, SLNs, NLCs, nanoemulsions) for various anti-TB drugs, ensuring optimal drug loading, stability, and release kinetics.
-
Enhanced Bioavailability Studies: Services to significantly improve the systemic and local bioavailability of your anti-TB compounds, overcoming solubility and absorption challenges.
-
Targeted Delivery Solutions: Development of ligand-conjugated delivery systems for precise delivery to macrophages, granulomas, or other specific cellular targets, maximizing therapeutic effect and minimizing off-target toxicity.
-
Sustained Release Formulations: Creation of delivery systems that provide prolonged drug release, enabling reduced dosing frequency and potentially improving patient adherence to lengthy TB regimens.
-
Pre-clinical Characterization: Comprehensive in vitro and in vivo characterization of delivery systems, including drug release profiles, cellular uptake, toxicity assessments, and efficacy studies in relevant TB models.
-
Scalability and Manufacturing Support: Expertise in developing scalable delivery systems manufacturing processes to facilitate seamless transition from research to clinical development.
Our commitment to scientific rigor, combined with state-of-the-art facilities and a collaborative approach, positions Creative Biolabs as your ideal partner in accelerating the development of more effective and safer TB treatments.
Connect with Our Experts Today
Workflow for Lipid-Based Drug Delivery Systems Development for TB
Published Data
Recent published data highlights the therapeutic potential of liposome-based vaccine strategies for TB. A study on the H56/CAF01 tuberculosis subunit vaccine demonstrated that a novel immunization strategy, involving subcutaneous prime and intrapulmonary boost, induced strong systemic and mucosal IgA and T-cell responses in mice. CAF01, a liposome-based cationic adjuvant, played a crucial role in potentiating these immune responses. This research underscores how liposomal formulations can effectively deliver vaccine components to target immune cells, leading to robust and protective immunity against M. tuberculosis. Such findings validate the use of lipid-based drug delivery systems in developing advanced TB vaccine candidates.
Creative Biolabs provide comprehensive delivery system development and both in vivo and in vitro validation services. Our expertise can assist customers in conducting cutting-edge research across multiple fields, including the diagnosis, treatment, and prevention of TB, accelerating the path from discovery to clinical application.
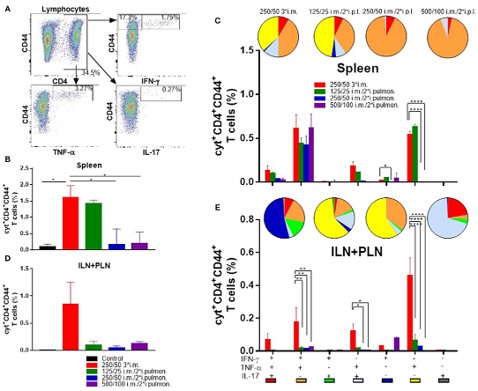 Fig. 4 H56/CAF01 prime-boost induces equivalent spleen T-cell responses via both routes.2,3
Fig. 4 H56/CAF01 prime-boost induces equivalent spleen T-cell responses via both routes.2,3
Creative Biolabs is dedicated to advancing the frontier of tuberculosis treatment through innovative lipid-based drug delivery systems. Our comprehensive services, from formulation development to targeted delivery strategies, are designed to address the most pressing challenges in anti-TB drug research. By partnering with us, you gain access to unparalleled expertise, cutting-edge technology, and a commitment to accelerating the development of life-saving therapies. We invite you to connect with our team of experts to discuss your specific project needs and explore how Creative Biolabs' solutions can empower your research.
Related Services
Resources
References
-
Kumar, Mahesh, et al. "Nanocarriers in tuberculosis treatment: challenges and delivery strategies." Pharmaceuticals 16.10 (2023): 1360. doi.org/10.3390/ph16101360.
-
Thakur, Aneesh, et al. "Dual-isotope SPECT/CT imaging of the tuberculosis subunit vaccine H56/CAF01: Induction of strong systemic and mucosal IgA and T-cell responses in mice upon subcutaneous prime and intrapulmonary boost immunization." Frontiers in immunology 9 (2018): 2825. doi:10.3389/fimmu.2018.02825.
-
Distributed under Open Access license CC BY 4.0, without modification.

For Research Use Only. Not For Clinical Use

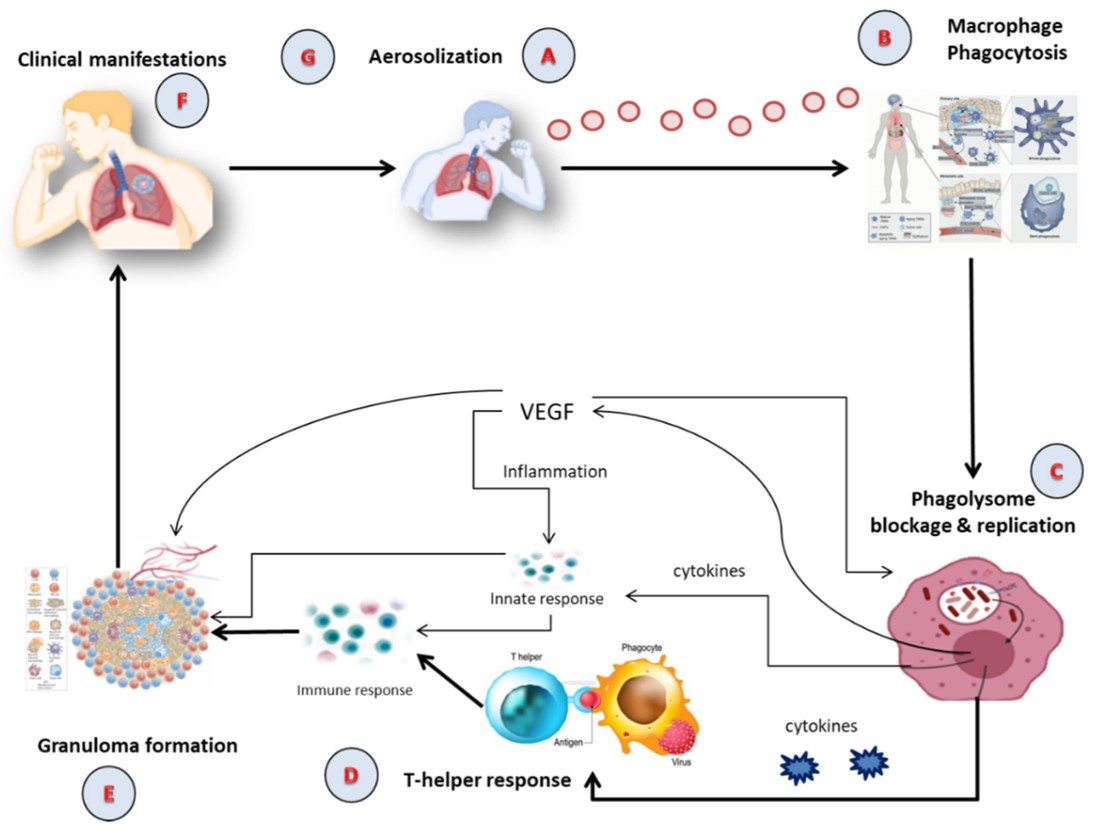 Fig. 1 The pathophysiology of active TB.1,3
Fig. 1 The pathophysiology of active TB.1,3
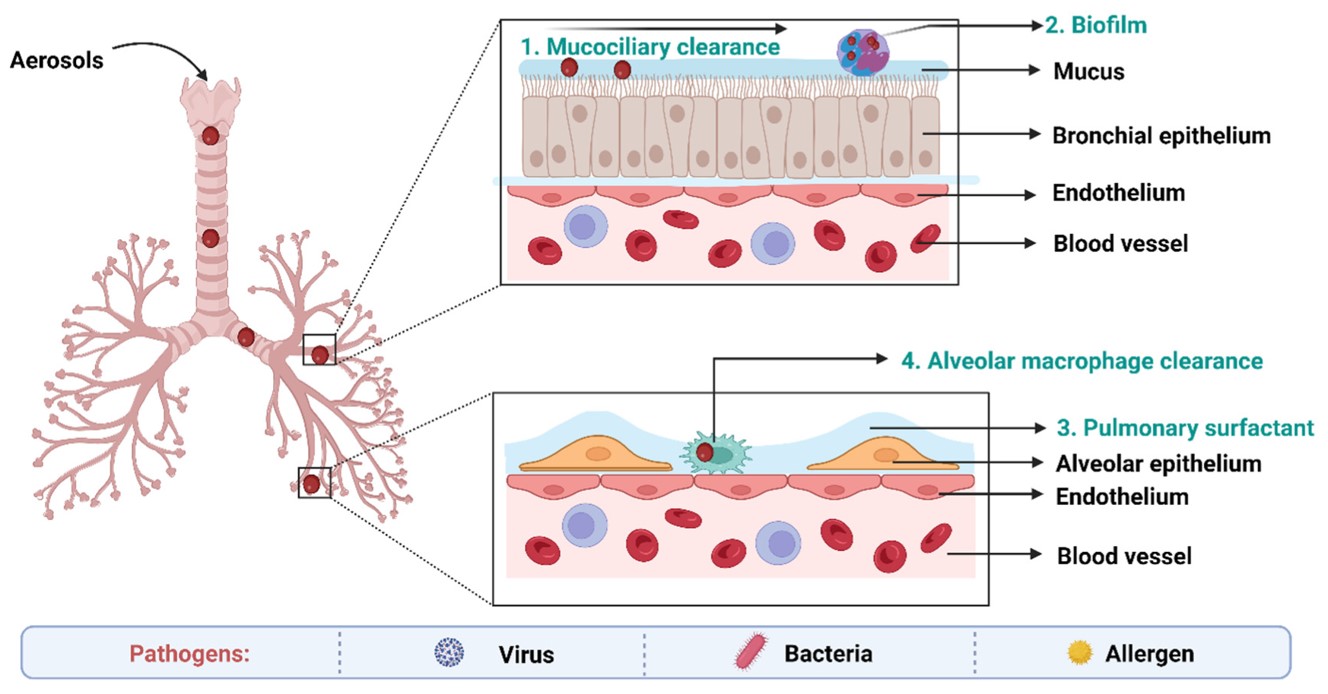 Fig. 2 Biological barriers in targeted drug delivery to lungs in TB.1,3
Fig. 2 Biological barriers in targeted drug delivery to lungs in TB.1,3
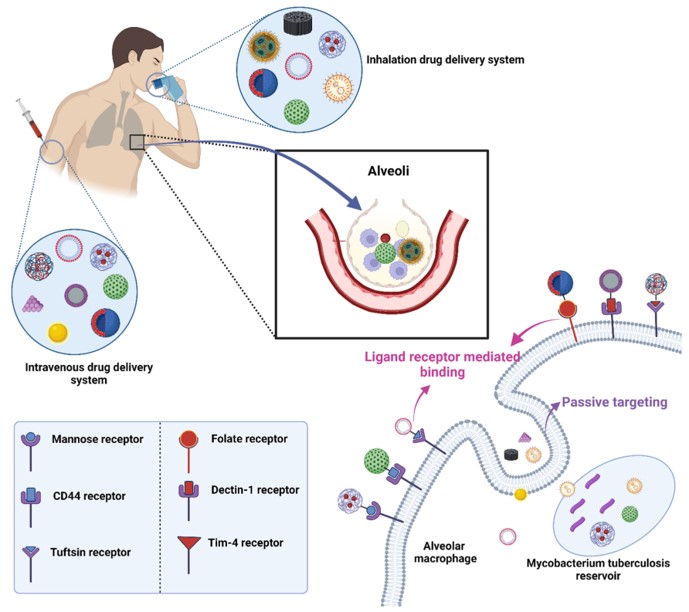 Fig. 3 Drug targeting employing conjugation of ligands with drug-loaded nanocarriers in TB.1,3
Fig. 3 Drug targeting employing conjugation of ligands with drug-loaded nanocarriers in TB.1,3
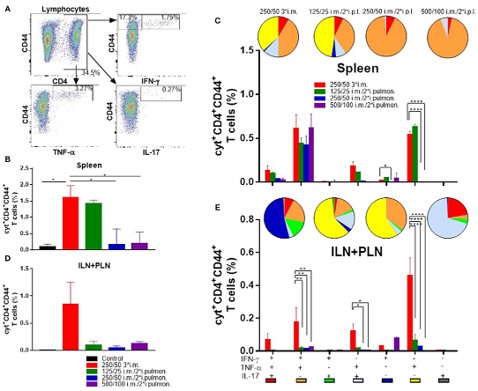 Fig. 4 H56/CAF01 prime-boost induces equivalent spleen T-cell responses via both routes.2,3
Fig. 4 H56/CAF01 prime-boost induces equivalent spleen T-cell responses via both routes.2,3



 For Research Use Only. Not For Clinical Use
For Research Use Only. Not For Clinical Use