Anti-Influenza Virus Glycan Shield Antibody Development Service
Influenza viruses have evolved sophisticated mechanisms to evade host immune defenses, most notably through the dense array of glycans on their surface glycoproteins. This phenomenon, known as the "glycan shield," presents a formidable barrier to neutralizing antibodies and complicates the development of a universal flu vaccine. At Creative Biolabs, we offer a specialized platform for developing high-affinity antibodies that target the glycosylated regions of the influenza hemagglutinin (HA). As part of our comprehensive Anti-Viral Glycan Shield Antibody Development service, we provide researchers with the precision tools needed to study viral antigenic variation, glycan-mediated immune evasion, and the structural basis of broad neutralization.
The Role of Glycans in Influenza Virus Immune Evasion
Structural Shielding by N-Glycans
The influenza virus hemagglutinin (HA) is a trimeric glycoprotein critical for viral entry, responsible for binding to sialic acid receptors on host cells and mediating membrane fusion. To protect its conserved functional sites—such as the receptor-binding site (RBS) on the head and the fusion machinery in the stem—the virus utilizes host cellular machinery to attach N-linked glycans to specific asparagine residues (e.g., Asn11, Asn28, Asn165, Asn285). These glycans form a physical "shield" that sterically hinders the access of neutralizing antibodies, effectively masking the underlying peptide epitopes from immune recognition.
The "Glycan Hole" Vulnerability
While the glycan shield is dense, it is rarely impervious. Gaps in the shield—termed "glycan holes"—often exist due to the specific spacing of N-linked glycosylation sequons. These holes expose the underlying protein surface to the immune system. Interestingly, some broadly neutralizing antibodies target these specific breaches. However, the virus often responds by mutating to "fill" these holes with new glycans, necessitating a continuous monitoring of glycan topology to predict viral escape.
Host-Specific Glycosylation Differences
A critical factor in vaccine development is the host cell machinery used for virus propagation. Influenza viruses grown in chicken eggs (a common vaccine production method) acquire different glycosylation patterns—often high-mannose or hybrid types—compared to the complex glycans found on viruses replicated in human respiratory cells. This mismatch can lead to "egg-adapted" antigenic changes, potentially reducing vaccine efficacy. Understanding these specific glycan differences is critical for designing better antigens.
Challenges in Antiviral Therapy Development
The positioning of these glycans is not static; the influenza HA evolves rapidly, adding or removing glycosylation sites to escape herd immunity—a process termed "glycan evolution." For researchers working on antiviral therapy and next-generation vaccines, this presents two major pain points:
- Epitope Masking: Conventional antibodies often fail to penetrate the dense glycan canopy, leading to low neutralization potency against heavily glycosylated strains.
- Steric Interference: Investigating the conserved stem region—a prime target for universal vaccines—is difficult because key epitopes are often protected by glycans at sites like Asn38 or Asn11, requiring antibodies that can accommodate or displace these sugars.
Custom Anti-Influenza Glycan Antibody Services
Creative Biolabs addresses these challenges through a robust custom antibody service specifically designed for the influenza glycan shield. We do not simply treat glycans as obstacles; we treat them as integral components of the epitope. Our platform allows for the generation of antibodies that either target the glycan-peptide interface (glycopeptide antibodies) or possess long CDR loops capable of penetrating the shield to reach conserved residues.
Targeted Development for HA Glycosylation Sites
We offer precise antibody development targeting specific glycosylation sites known to modulate antigenicity, such as the conserved glycan at Asn11 (stem) or variable glycans on the globular head (e.g., Asn165 in H3N2). By using site-specifically glycosylated immunogens, we isolate clones that recognize the distinct topography of the shielded virus.
Broadly Neutralizing Antibody (bnAb) Discovery
Supporting the quest for a universal flu vaccine, we screen for "glycan-tolerant" antibodies. These rare antibodies bind to conserved epitopes (like the HA stem) regardless of the surrounding glycan density, or utilize the glycan itself as an anchor point for higher affinity binding.
Subtype-Specific Solutions (H1N1, H3N2, B)
Our service covers major seasonal and pandemic strains. We generate reagents specific for the glycan profiles of H1N1, H3N2, and Influenza B viruses. This is crucial for pre-clinical profiling, as glycosylation patterns differ significantly between subtypes and even between egg-grown vs. cell-grown vaccine stocks.
Glycan Occupancy and Resistance Analysis
Beyond antibody generation, we provide analytical services to assess how specific glycan mutations affect antibody binding. This data helps researchers predict potential escape mutants and evaluate the "fitness cost" of new glycosylation sites on viral replication.
Project Workflow
Request a Quote for Influenza Antibody Service
Why Choose Our Influenza Glycan Services?
Native Conformation Focus
Immunogens are engineered to present the correct quaternary structure of HA, ensuring antibodies recognize the native trimer.
Universal Vaccine Ready
Specialized screening for antibodies that target the highly conserved, glycan-protected stem region.
Comprehensive Data
Full characterization including EC50 values, epitope binning, and cross-reactivity profiles against multiple strains.
Expert Consultation
Ph.D. level scientists guide your project from antigen design to final validation, ensuring relevance to your viral model.
Published Data
Recent breakthrough research has illuminated the potential of anti-carbohydrate antibodies in targeting the evolving influenza glycan shield. A pivotal study published in PLOS Pathogens by Lee et al. (2021) demonstrated that the broadly neutralizing antibody 2G12, originally isolated from HIV-1 patients, possesses remarkable cross-neutralizing activity against human seasonal H3N2 influenza viruses isolated over the past three decades. By employing advanced liquid chromatography-mass spectrometry (LC-MS) and negative-stain electron microscopy (nsEM), the researchers revealed that H3N2 viruses have evolved a dense cluster of under-processed oligomannose-type glycans on the hemagglutinin (HA) globular head, specifically centered around the conserved residue N165 and the evolutionarily acquired residue N246.
The published data indicates that 2G12 neutralizes these viruses by specifically recognizing this high-mannose cluster, which is located proximal to the viral receptor-binding site (RBS). Mutational analysis confirmed that both N165 and N246 are critical for viral fitness and antibody sensitivity. Furthermore, structural characterization visualized distinct antibody binding modes—specifically a lateral interaction where the antibody bridges glycans on the same protomer—which appears essential for effective neutralization. These findings provide a structural proof-of-concept that the viral "glycan shield," often considered merely a barrier to immune recognition, contains conserved vulnerabilities that can be exploited for the development of novel antiviral therapeutics and universal vaccine strategies.
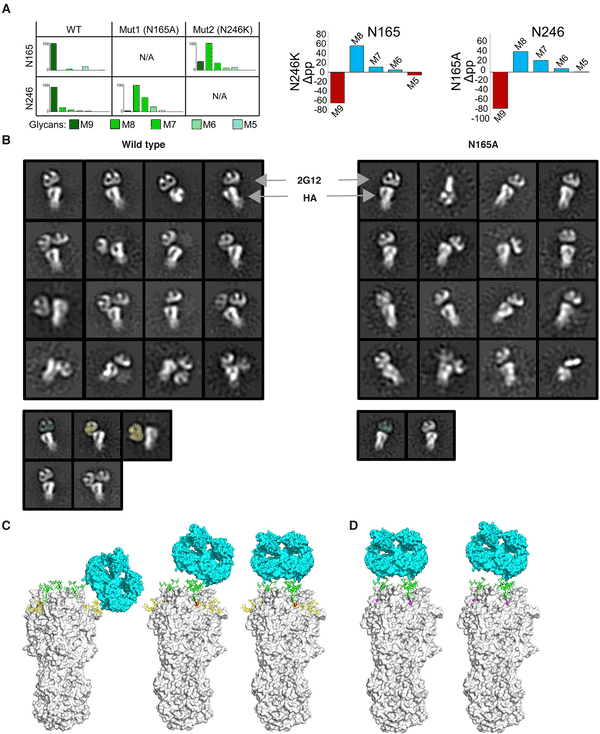 Fig.1 Structural Basis of 2G12 Antibody Neutralization Targeting the Influenza H3N2 Glycan Shield.1
Fig.1 Structural Basis of 2G12 Antibody Neutralization Targeting the Influenza H3N2 Glycan Shield.1
FAQs
How do you ensure the antibody recognizes the native viral trimer and not just the recombinant protein?
We utilize trimer-stabilized immunogens (e.g., foldon-tagged HA) during both immunization and screening. We also validate final clones using assays that require native conformation, such as Hemagglutination Inhibition (HAI) assays and flow cytometry on HA-transfected cells.
Can you generate antibodies that distinguish between different glycosylation states of the same HA?
Yes. By employing differential screening strategies—using fully glycosylated HA versus deglycosylated or glycan-mutant HA variants—we can isolate antibodies that are sensitive to the presence or absence of specific glycan chains.
Do you offer services for Influenza B virus in addition to Influenza A?
Yes, our custom antibody service encompasses both Influenza A (Group 1 and Group 2) and Influenza B lineages (Victoria and Yamagata). We can target the distinct glycosylation patterns found on the HA of Influenza B viruses.
Is this service suitable for developing universal flu vaccine candidates?
While our service focuses on generating research reagents, the antibodies we develop are invaluable tools for universal flu vaccine research. They can serve as positive controls for broadly neutralizing epitopes, structural probes for immunogen design, or reagents to map conserved sites on the HA stem.
What is the typical timeline for a custom anti-influenza glycan antibody project?
A standard project typically takes 4–6 months, depending on the complexity of the antigen and the host species selected. We provide a detailed Gantt chart at the start of the project and regular bi-weekly updates to keep you informed of progress.
Can you test the antibodies for cross-reactivity against recent seasonal strains?
Yes. We can include a cross-reactivity panel in the validation phase, testing the antibodies against a diverse array of recombinant HAs from recent H1N1, H3N2, and B strains to determine the breadth of binding.
What Our Customers Say
"The 'glycan shield' has always been a major hurdle in our structural biology work. Creative Biolabs generated a Fab fragment that not only bound the HA stem but actually stabilized the trimer for Cryo-EM. The specificity for the glycosylated epitope was remarkable."
"We needed a panel of antibodies to map antigenic drift in H3N2 strains over the last decade. Their team designed a custom library approach that successfully identified clones sensitive to single glycan additions. This data is crucial for our vaccine efficacy studies."
"Developing reagents for antiviral therapy research is tough when targets are masked by sugars. The antibodies delivered by Creative Biolabs showed excellent breadth of binding across group 1 influenza viruses. A highly professional service."
"I was impressed by their consultation phase. They clearly understood the implications of HA stem glycosylation on our universal vaccine design. The final antibodies were well-characterized and worked perfectly in our neutralization assays."
Reference:
- Lee, C. D., et al. "A cross-neutralizing antibody between HIV-1 and influenza virus." PLOS Pathogens 17.3 (2021): e1009407. Distributed under Open Access license CC BY 4.0. https://doi.org/10.1371/journal.ppat.1009407
