Dental Disease related Glycan Introduction
Accelerate Your Glycan-Based Discoveries!
Are you currently facing challenges in understanding complex disease mechanisms, identifying novel biomarkers, or developing highly specific therapeutic interventions in oral health? Creative Biolabs' Glycan in Dental Disease services help you accelerate research and development, obtain high-quality glycan insights, and develop targeted solutions through advanced glycomics and glycobiological analysis. We empower your projects with unparalleled precision and depth.
Contact our team to get an inquiry now!
Introduction
Periodontitis, often referred to as periodontal disease, constitutes a widespread oral disorder marked by inflammatory destruction of periodontal structures. During its initial stage (gingivitis), this disorder manifests as marked by gum inflammation, redness, and potential bleeding. When progressing to advanced periodontitis, tissue detachment from teeth occurs, accompanied by bone degradation and potential tooth loss. The pathology primarily stems from bacterial colonization in oral tissues, infiltrating periodontal structures. Contributing factors encompass tobacco use, diabetes mellitus, immunodeficiency conditions, genetic predisposition, and specific pharmacological treatments. Diagnosis typically involves clinical evaluation of gingival status using visual inspection, periodontal probing, and radiographic assessment of alveolar bone levels. Therapeutic approaches integrate intensified home hygiene protocols with periodontal debridement. Epidemiologically, around 50% of Americans aged 30+ experience some disease manifestation, escalating to 70% in those over 65, with higher prevalence observed in males versus females.
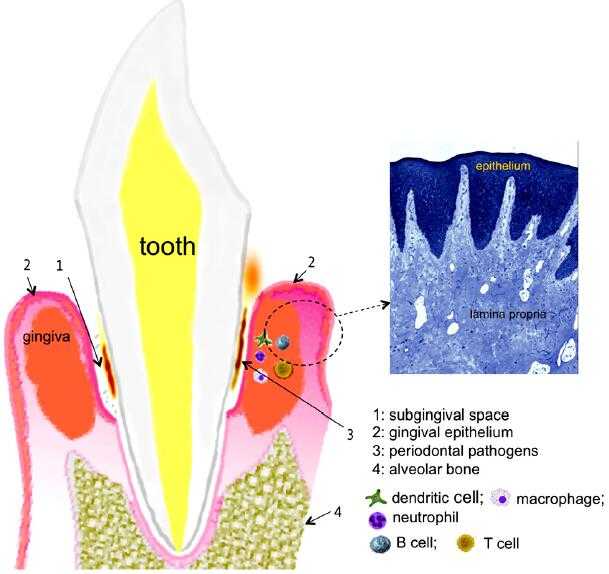 Fig.1 N-glycosylation associated with risk factors for dyslipidemia.1,3
Fig.1 N-glycosylation associated with risk factors for dyslipidemia.1,3
The Role of Glycans in Dental Disease
The human oral cavity harbors a complex microbial ecosystem, housing approximately 700 bacterial species spanning diverse taxonomic groups. Within this community, specific gram-negative anaerobic species forming subgingival biofilm matrices induce periodontitis – a prevalent inflammatory disorder. Notably, the bacterial consortium termed the "red complex" (Porphyromonas gingivalis, Treponema denticola, and Tannerella forsythia) are primary contributors to periodontal pathogenesis. Emerging evidence demonstrates that T. forsythia and P. gingivalis employ protein glycosylation mechanisms to subvert host immune defenses, facilitating persistent colonization and subsequent tissue degradation.
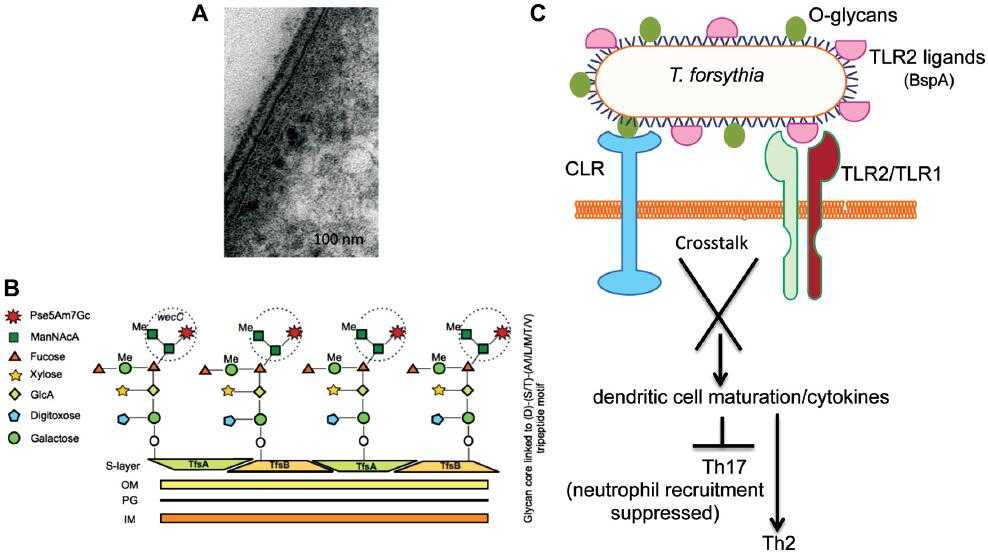 Fig.2 Schematic diagram of the O-glycan core structure linked to a peptide motif in Tannerella surface-layer proteins and signaling crosstalk between a C-type lectin-like receptor (CLR) and TLR2 activated by O-glycans and TLR2 ligands, respectively.1,3
Fig.2 Schematic diagram of the O-glycan core structure linked to a peptide motif in Tannerella surface-layer proteins and signaling crosstalk between a C-type lectin-like receptor (CLR) and TLR2 activated by O-glycans and TLR2 ligands, respectively.1,3
Protein modification with complex glycans is increasingly identified across numerous pathogenic and commensal bacteria, proving critical for their successful adaptation within hosts. Specifically, viridans group streptococci implicated in caries and gingivitis produce serine-rich proteins requiring O-glycosylation stability. These microbes also possess binding domains recognizing O-linked sialoglycans or oral mucins to facilitate mucosal cell adherence. If introduced into circulation during dental interventions, identical binding proteins identify platelet glycoproteins like GPIb-α, transporting bacteria to damaged cardiac valves and causing severe bacterial endocarditis. Further studies revealed that surface glycans of periodontal pathogens coordinate dendritic cell cytokine profiles to direct T cell responses, enabling microbial persistence and inducing periodontal inflammation. Additionally, surface carbohydrates may shield certain periodontal bacteria from serum complement or aid immune evasion through molecular mimicry. Consequently, pathogen glycans represent promising targets for treating oral diseases.
Published Data
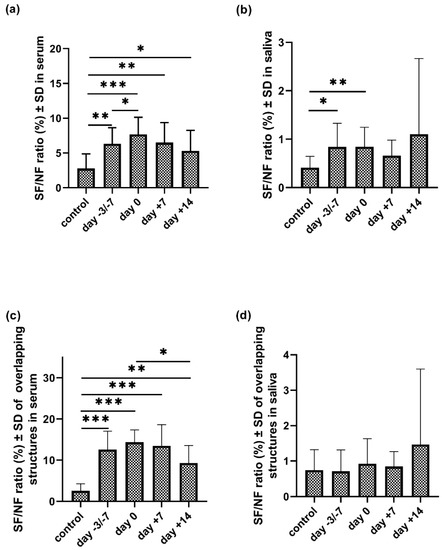 Fig.3 Principal component analysis of serum (a) and salivary (b) IgA N-glycosylation profiles from controls and four APSC stages.2,3
Fig.3 Principal component analysis of serum (a) and salivary (b) IgA N-glycosylation profiles from controls and four APSC stages.2,3
The study investigated the total N-glycans of serum and salivary IgA from patients undergoing autologous peripheral stem-cell transplantation (APSCT) at four distinct stages, comparing them to healthy controls. Capillary electrophoresis detected 31 serum and 38 salivary N-glycan structures. A key finding was that 14 of the serum glycan structures and 6 of the salivary glycan structures exhibited significant changes when compared to the control group, indicating a systemic and local immune response to transplantation. Specifically, the sialoform to neutral (SF/NF) carbohydrate ratio in serum was significantly elevated across all examined APSCT stages compared to controls. This suggests an increase in sialylated glycans, often associated with inflammatory processes or immune modulation. The salivary IgA N-glycome profile was also found to reflect the impact of APSCT on local oral immunity. Furthermore, the study noted that the highly variable cariological and periodontal status, along with person-specific oral flora, could further influence the glycosylation patterns of secreted salivary IgA. This corroborates prior findings of serum and gingival crevicular fluid (GCF) IgG hypogalactosylation during periodontitis progression, highlighting glycans' significant relationship with oral health.
What We Can Offer?
Creative Biolabs leverages its extensive experience and cutting-edge technology to provide a comprehensive suite of services focused on Glycan in Dental Disease, designed to meet the diverse needs of our clients.
- Oral Sample Glycan Profiling
- Bacterial Glycosylation Analysis
- Anti-Glycan Antibody Development
- Glyco-Biomarker Discovery & Validation
- Host-Pathogen Glycan Interaction Studies
- Custom Glycosylation Studies
Discover the Creative Biolabs Edge – Obtain Your Pricing Now
Why Choose Us?
Choosing Creative Biolabs for your Glycan in Dental Disease research means partnering with a leader in glycobiology, committed to delivering exceptional results and unparalleled scientific support.
- Unrivaled Expertise: Over years of specialized experience in glycobiology and dental research.
- Cutting-Edge Technology: Access to state-of-the-art glycomics platforms for high-resolution analysis.
- Comprehensive Solutions: From sample preparation to advanced data interpretation and strategic recommendations.
- Customized Approach: Tailored services to meet the unique requirements of each research project.
- Actionable Insights: Delivering meaningful data that translates directly into diagnostic and therapeutic advancements.
FAQs
Here are some common scientific questions about glycan analysis in dental disease research.
Q: What are the primary applications of glycan analysis in understanding oral infectious diseases?
A: Glycan analysis is crucial for understanding how pathogens adhere to host cells and evade the immune system. It helps identify specific glycan targets for anti-adhesion therapies, unravel mechanisms of biofilm formation, and discover novel biomarkers for disease progression and diagnosis in conditions like periodontitis and dental caries.
Q: How does the analysis of bacterial glycans contribute to the development of new dental therapeutics?
A: By characterizing bacterial surface glycans, researchers can identify critical virulence factors and immune modulators. This knowledge is instrumental in designing targeted therapeutics, such as specific inhibitors of glycan-mediated interactions, or in developing vaccines that disrupt bacterial colonization and pathogenicity in the oral cavity.
Q: What level of detail can glycan analysis provide regarding the structure and function of glycans in oral samples?
A: Advanced glycan analysis, particularly using high-resolution mass spectrometry, can provide extremely detailed information about glycan structures, including their composition, branching patterns, and linkages. This depth of information is essential for correlating specific glycan motifs with biological functions or disease states.
Related Products and Services
To further advance your glycobiology R&D, we provide a portfolio of solutions:
- Monoclonal Antibodies
- Polyclonal Antibodies
- Secondary & Tag Antibodies
- Isotype & Loading Control Antibodies
- Carbohydrate Antigens
Creative Biolabs also provides related services, click the buttons to find more details.
To explore these capabilities, please contact us for more information.
References:
- Settem, Rajendra P et al. "Protein-linked glycans in periodontal bacteria: prevalence and role at the immune interface." Frontiers in microbiology vol. 4 310. 17 Oct. 2013, https://doi.org/10.3389/fmicb.2013.00310
- Gebri, Enikő et al. "N-Glycosylation Alteration of Serum and Salivary Immunoglobulin a Is a Possible Biomarker in Oral Mucositis." Journal of clinical medicine vol. 9,6 1747. 5 Jun. 2020, https://doi.org/10.3390/jcm9061747
- Distributed under Open Access license CC BY 4.0, without modification.
