SARS-CoV-2 Spike Protein Glycosylation and Neutralization
The ongoing battle against COVID-19 has placed the SARS-CoV-2 spike protein at the center of global research efforts. As the primary machinery for viral entry, the spike protein is heavily modified by host-derived glycans, which facilitate immune evasion and stabilize its metastable prefusion conformation. Understanding the intricacies of sars-cov-2 spike glycosylation is essential for the design of effective therapeutics and vaccines. At Creative Biolabs, we leverage our advanced glyco-analytical platforms to decipher the "glycan shield" of coronaviruses, offering specialized solutions such as our Anti-Coronavirus Glycan Shield Antibody Development service. We assist researchers in characterizing glycan occupancy, mapping epitope accessibility, and developing neutralizing antibodies that can penetrate this formidable defense.
The Structural Biology of the Spike Glycoprotein
The SARS-CoV-2 spike (S) protein is a large, trimeric Class I fusion protein that protrudes from the viral envelope. It is synthesized as a precursor (S0) and cleaved by furin-like proteases into two subunits: S1, which contains the receptor-binding domain (RBD), and S2, which drives membrane fusion. Each protomer within the trimer possesses 22 N-linked glycosylation sites, resulting in a dense coating of 66 glycans per trimer.
Unlike the "silent" shield of HIV-1, which is predominantly composed of high-mannose glycans, the sars-cov-2 spike glycosylation profile is more heterogeneous. Mass spectrometry analysis reveals a mixture of complex, hybrid, and oligomannose-type glycans. While this shield is less dense than that of HIV, it is strategically positioned to mask conserved epitopes without hindering the flexibility required for the RBD to engage the host receptor. This sophisticated arrangement allows the virus to hide its immunogenic surfaces from covid-19 neutralizing antibodies while maintaining full functionality.
Glycan Shielding and Immune Evasion
The concept of glycan masking is a critical evolutionary strategy for enveloped viruses. By coopting the host's glycosylation machinery, SARS-CoV-2 coats its surface proteins with "self" sugars, which are generally tolerated by the human immune system. This steric occlusion prevents the maturation of high-affinity B cell responses against the underlying protein peptide backbone.
Detailed structural studies utilizing cryo-electron microscopy (cryo-EM) and molecular dynamics simulations have shown that glycans at specific sites, such as N165, N234, and N343, play pivotal roles beyond simple shielding. They form a regulatory gate that modulates the conformational dynamics of the RBD. For instance, the glycan at N234 fills a vacancy created when the RBD lifts up, stabilizing the "open" state required for receptor binding. Conversely, removing these glycans can collapse the RBD into a "closed" state, potentially altering the virus's infectivity and susceptibility to neutralization.
Epitope Masking
Glycans physically cover conserved protein epitopes, preventing antibody access and reducing neutralization potency.
Conformational Control
Specific N-glycans act as structural latches, stabilizing the RBD in the "up" conformation necessary for ACE2 engagement.
Antigenic Drift
Mutations that introduce or remove glycosylation sites can rapidly alter the antigenic landscape, leading to variant escape.
Diversity of N-Glycans Across the Spike Trimer
The distribution of glycan types across the SARS-CoV-2 spike protein is not random; rather, it reflects the spatial constraints and accessibility of each site to glycan-processing enzymes in the Golgi apparatus. The S1 subunit, particularly the N-terminal domain (NTD) and RBD, exhibits a higher proportion of complex-type glycans, suggesting these regions are exposed and accessible. In contrast, the S2 subunit and the stem regions are populated by under-processed oligomannose-type glycans, indicative of steric crowding that restricts enzymatic access. Understanding these site-specific profiles is crucial for designing immunogens that faithfully mimic the viral surface.
| Glycosylation Site | Predominant Glycan Type | Structural & Functional Role |
|---|---|---|
| N165 | Complex | Modulates the dynamic "up/down" transition of the Receptor Binding Domain (RBD). |
| N234 | Oligomannose (Man9) | Functions as a structural "kickstand," filling the void left by the RBD in the "up" state to stabilize receptor binding competence. |
| N343 | Complex | Essential for the opening mechanism of the RBD; loss of this glycan significantly reduces ACE2 binding capacity. |
| N616, N657 | Oligomannose | Located near the S1/S2 cleavage site; may influence proteolytic processing and subsequent viral fusion. |
| N1158, N1173, N1194 | Complex | Situated on the stalk of the S2 subunit; provide extensive shielding for the fusion machinery. |
The Emerging Importance of O-Linked Glycosylation
While N-linked glycans dominate the SARS-CoV-2 glycan shield, recent high-sensitivity mass spectrometry studies have identified occupied O-linked glycosylation sites, particularly around the S1/S2 cleavage site and the hinge regions. Although O-glycans are less abundant, their presence can have profound effects on viral biology due to their strategic location.
- Regulation of Proteolysis: O-glycans located near the furin cleavage site (residues 681-685) can physically obstruct protease access. This modulation of cleavage efficiency directly impacts viral fusion and infectivity, as uncleaved spike proteins are less efficient at mediating cell entry.
- Hinge Flexibility: O-glycosylation adds rigidity to the peptide backbone. The presence of O-glycans in the hinge regions connecting the RBD to the rest of the spike can restrict conformational freedom, potentially locking the RBD in specific states that favor or hinder neutralization.
- Variant-Specific Patterns: Emerging variants of concern (VOCs) often exhibit mutations near O-glycosylation sites. For example, mutations in the N-terminal domain or near the furin cleavage site can create or destroy O-linked sequons, suggesting that modulation of O-glycosylation is a mechanism of viral evolution and adaptation.
Impact on ACE2 Binding and Neutralization
Modulation of Receptor Affinity
The interaction between the SARS-CoV-2 RBD and the human Angiotensin-Converting Enzyme 2 (ACE2) receptor is the first step of infection. Research indicates that the glycan at N90 on ACE2 and glycans on the viral spike influence this binding affinity. While glycosylation is not strictly required for binding, the removal of specific glycans can modulate the kinetics of the interaction. sars-cov-2 spike glycosylation ensures the RBD is presented in a favorable orientation, optimizing ace2 binding despite the dense carbohydrate layer.
Implications for Therapeutic Antibodies
Most potent covid-19 neutralizing antibodies target the RBD. However, the efficacy of these antibodies is heavily dependent on the glycan occupancy of the spike protein. "Glycan holes"—areas where the shield is incomplete due to structural constraints—represent vulnerable targets. Furthermore, some broad-spectrum neutralizing antibodies have evolved to accommodate or even utilize glycans for binding, interacting with both the peptide and the carbohydrate moieties. Understanding the detailed spike protein structure and its glycan coverage is therefore crucial for selecting monoclonal antibodies that remain effective across different viral variants.
Our Solutions for Coronavirus Research
Creative Biolabs provides a comprehensive suite of services designed to accelerate your research into viral glycoproteins. We combine structural biology, glycomics, and immunology to deliver actionable insights.
Glycan Shield Analysis & Mapping
We utilize high-resolution mass spectrometry and cryo-EM to map the site-specific glycosylation of coronavirus spike proteins. Our reports detail glycan composition (high-mannose vs. complex), occupancy rates, and micro-heterogeneity, helping you visualize the glycan shield with precision.
Custom Glycosylation of Viral Antigens
Recombinant expression systems often yield non-native glycosylation patterns. We offer Custom Glycosylation of Biomolecules to produce spike protein trimmers with human-like glycan profiles, ensuring that your binding assays and immunization studies reflect the true viral surface.
Epitope Mapping & Specificity Profiling
Using our advanced Glycoarray Platforms, we screen antibody candidates against diverse glycan and glycopeptide libraries. This allows us to identify antibodies that bind specifically to glycan-dependent epitopes or broad-spectrum antibodies that penetrate the shield.
Neutralizing Antibody Development
From phage display to hybridoma technology, we generate high-affinity monoclonal antibodies targeting the RBD, NTD, and S2 subunits. We test candidates for neutralization potency using pseudovirus and live-virus assays, specifically assessing their ability to overcome glycan masking.
Request a Quote for Spike Protein Services
Published Data
Recent site-specific mass spectrometric analysis has provided a comprehensive benchmark of the N-linked glycan arrangement on the trimeric SARS-CoV-2 spike protein. This structural characterization reveals that each protomer contains 22 N-linked glycosylation sites, which are occupied by a heterogeneous mixture of oligomannose, hybrid, and complex-type glycans. Unlike the dense "mannose patch" shields observed on HIV-1 Env or Lassa virus GPC, the SARS-CoV-2 glycan shield is less dense, comprising approximately 28% oligomannose-type glycans. This suggests that while the viral surface is camouflaged, it may exhibit more vulnerabilities to neutralizing antibodies than other class I fusion proteins. Crucially, the study maps specific glycans, such as N165, N234, and N343, to the receptor-binding domain (RBD), demonstrating their role in shielding the receptor-binding motif and modulating the RBD's "up" and "down" conformational dynamics. Furthermore, the analysis confirms that the N-linked glycans are distributed across both the S1 and S2 subunits, with under-processed oligomannose clusters protecting structurally constrained regions. These findings are pivotal for immunogen engineering, as they highlight the necessity of replicating native-like glycosylation patterns to elicit potent neutralizing responses and avoid distracting non-native epitopes in vaccine candidates.
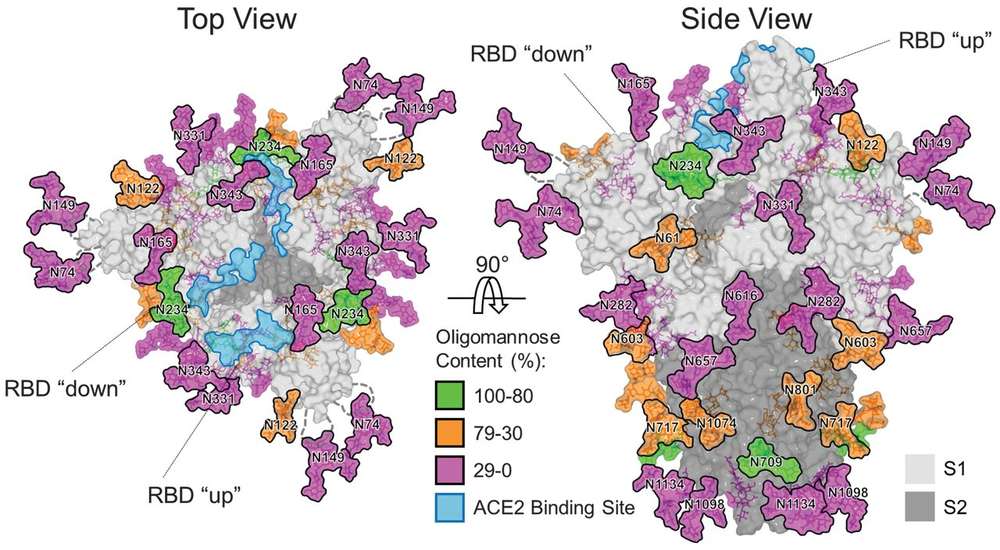 Fig.1
Structure-based mapping of SARS-CoV-2 S N-linked glycans.1
Fig.1
Structure-based mapping of SARS-CoV-2 S N-linked glycans.1
FAQs
Why is the glycosylation of the SARS-CoV-2 spike protein important for vaccine development?
Glycosylation affects the protein's folding, stability, and antigenicity. Since glycans can mask immunogenic epitopes, vaccines must present the spike protein with a native-like glycan profile to elicit antibodies that can recognize the actual virus. Incorrect glycosylation in vaccine antigens can lead to the production of non-neutralizing antibodies.
Does SARS-CoV-2 have a denser glycan shield than HIV?
No, SARS-CoV-2 generally has a less dense glycan shield compared to HIV-1. While it is heavily glycosylated, there are more exposed protein surfaces ("glycan holes") on the SARS-CoV-2 spike, which may explain why neutralizing antibodies are generated more readily against COVID-19 than HIV.
How does Creative Biolabs analyze spike protein glycosylation?
We employ a combination of Liquid Chromatography-Mass Spectrometry (LC-MS/MS) for site-specific glycan analysis and glycopeptide mapping. We also use glycan array screening to assess the binding specificity of antibodies against viral glycans.
Can you develop antibodies that target specific glycan epitopes on the spike protein?
Yes. Through our specialized Anti-Coronavirus Glycan Shield Antibody Development service, we can isolate and engineer antibodies that target specific glycan-dependent epitopes or regions where glycans are integral to the antibody-antigen interface.
Does the glycan profile change between different SARS-CoV-2 variants?
Yes, mutations in the spike gene can add or remove N-linked glycosylation sites (sequons). These changes can alter the glycan shield, potentially affecting immune recognition and neutralizing antibody efficiency. Monitoring these changes is a key part of variant surveillance.
Reference:
- Watanabe, Yasunori, et al. "Site-specific glycan analysis of the SARS-CoV-2 spike." Science 369.6501 (2020): 330-333. Distributed under Open Access license CC BY 4.0. https://doi.org/10.1126/science.abb9983
Supports
- Anti-Coronavirus Glycan Shield Antibody Development
- Glycoarray Platforms
- Glycosylation Analysis
- Custom Glycosylation of Biomolecules
