Anti-Glomerular Basement Membrane (GBM) Nephritis Modeling & Pharmacodynamics Service
Creative Biolabs offers a variety of well-established models to evaluate the therapeutic efficacy of potential treatments for anti-GBM nephritis, ensuring robust and reliable research outcomes for preclinical studies.
Introduction
Anti-glomerular basement membrane (GBM) nephritis is a rare and severe autoimmune kidney disorder caused by the formation of autoantibodies targeting the glomerular basement membrane. This autoimmune response leads to the rapid development of glomerulonephritis, which results in glomerular inflammation, crescent formation, and progressive renal dysfunction. The disease often presents with symptoms of nephritic syndrome, including hematuria, proteinuria, and hypertension. If left untreated, anti-GBM nephritis can rapidly progress to kidney failure and end-stage renal disease. It is frequently associated with other autoimmune conditions, such as Goodpasture syndrome, which also affects the lungs. Early diagnosis, typically through the detection of anti-GBM antibodies in the blood and kidney biopsy, is critical for initiating appropriate treatment. Immunosuppressive therapies, such as corticosteroids and cyclophosphamide, are commonly used to manage the disease and prevent further renal damage. Given the severity and rapid progression of anti-GBM nephritis, preclinical models are vital for evaluating new treatments and understanding the underlying pathophysiology.
Anti-Glomerular Basement Membrane (GBM) Nephritis Model
The anti-GBM nephritis model is established by immunizing rodents with anti-GBM serum. This induces a condition resembling human anti-GBM nephritis, with histological features such as glomerular inflammation and crescent formation. The model is characterized by its ability to reproduce the clinical and pathological manifestations of the disease, including proteinuria, hematuria, and renal dysfunction. The advantages of this model include its high reproducibility and ability to mimic the rapid progression of the disease seen in humans. However, one limitation is that it may not fully replicate the chronic nature of the disease observed in some human cases. It is widely used for the testing of novel therapies and understanding the underlying pathogenesis of anti-GBM nephritis.
- Simulates: This model simulates autoimmune kidney disease, specifically anti-GBM nephritis, by inducing the formation of anti-GBM antibodies in rodents, resulting in glomerular injury and renal inflammation. The model effectively mimics the acute, rapidly progressive nature of the human disease.
- Evaluates Drugs: The anti-GBM nephritis model is used to evaluate potential therapeutic agents for autoimmune kidney diseases. It helps in testing the efficacy of immunosuppressive drugs, such as corticosteroids and cyclophosphamide, as well as novel biologics targeting specific immune pathways. The model is ideal for assessing treatments aimed at reducing glomerular inflammation, preventing kidney damage, and improving renal function.
Evaluation Platform
- Animals: Mouse, Rat.
-
Measurements
We offer a variety of measurements for evaluating drug efficacy in anti-GBM nephritis models, utilizing an array of advanced technologies, including but not limited to:- General observations: Body weight, renal function (serum creatinine, blood urea nitrogen), and survival rate.
- Urinalysis: Proteinuria and hematuria levels.
- Histopathology: Assessment of glomerular injury, crescent formation, and immune cell infiltration using H&E staining and immunohistochemistry.
- Cytokine profiling: Levels of inflammatory mediators such as TNF-α, IL-6, and IL-1β using ELISA.
- Gene/protein expression profiling: RT-PCR and Western blot for markers of renal inflammation and fibrosis, such as MCP-1, ICAM-1, and collagen IV.
- Immunohistochemistry: Detection of glomerular immune deposits and cell infiltration, including T-cells, macrophages, and neutrophils.
In addition to our established models, our scientific team provides personalized experimental design, model selection, and data analysis to ensure the most effective and customized approach for your research.
Related Services
In addition to the anti-GBM nephritis model, we also provide various autoimmune nephropathy models. These models offer additional insights into autoimmune-mediated kidney damage and are valuable for evaluating a broader spectrum of therapeutic strategies.
- Thy-1 Nephritis Model
- Fx1A Nephritis Model
- IgA Nephropathy Model
- Spontaneous Systemic Lupus Erythematosus (SLE) Model
- Systemic Lupus Erythematosus Induced Model
Our advantages
- Comprehensive model options: We provide a range of preclinical models tailored to different stages and severities of anti-GBM nephritis.
- Customizable research support: Our team assists with experimental design, data analysis, and model customization to meet specific research needs.
- Expertise in autoimmune diseases: Our company specializes in autoimmune nephropathy models, ensuring an in-depth understanding and accurate results.
- High reproducibility: Our models are highly reproducible, ensuring consistent and reliable data for preclinical research.
- Cutting-edge technology: We use advanced technologies such as multi-omics, histopathology, and cytokine profiling to provide a comprehensive evaluation of therapeutic interventions.
Work with Us
- Summarize the project requirements and fill in the information collection form.
- Sign a CDA from both parties to further communicate information, such as targets.
- Select an animal model, discuss experimental design, and determine assay parameters.
- Project costing and project schedule forecasting.
- We provide a detailed project plan, including the required sample quantities, methods, and protocols.
- Both parties confirm the project details and start the project.
- Confirm the timeline of the project.
- We provide periodic results and information on the animal's condition.
- We will work together to make project adjustments as necessary.
- We provide a comprehensive project report promptly.
- We arrange transportation for the produced samples.
- We provide a discussion of the project results and help to arrange the next steps.
- Data storage and archiving.
FAQs
-
1. What is the primary use of the anti-GBM nephritis model?
This model is used for preclinical testing of therapies aimed at autoimmune kidney diseases, particularly anti-GBM nephritis.
-
2. How long does it take to establish the model?
The model typically takes 3-4 weeks to develop after immunization with the anti-GBM peptide.
-
3. Can the model be used for long-term studies?
While the model is primarily used for acute studies, it can be adapted for chronic studies with appropriate modifications.
-
4. What types of drugs can be tested with this model?
This model is suitable for testing immunosuppressive agents, biologics, and other therapies targeting the immune system to reduce kidney inflammation.
-
5. Are there any limitations to this model?
The main limitation is that it may not fully replicate the chronic progression of anti-GBM nephritis in all cases. However, it accurately mimics the acute phase of the disease.
Published Data
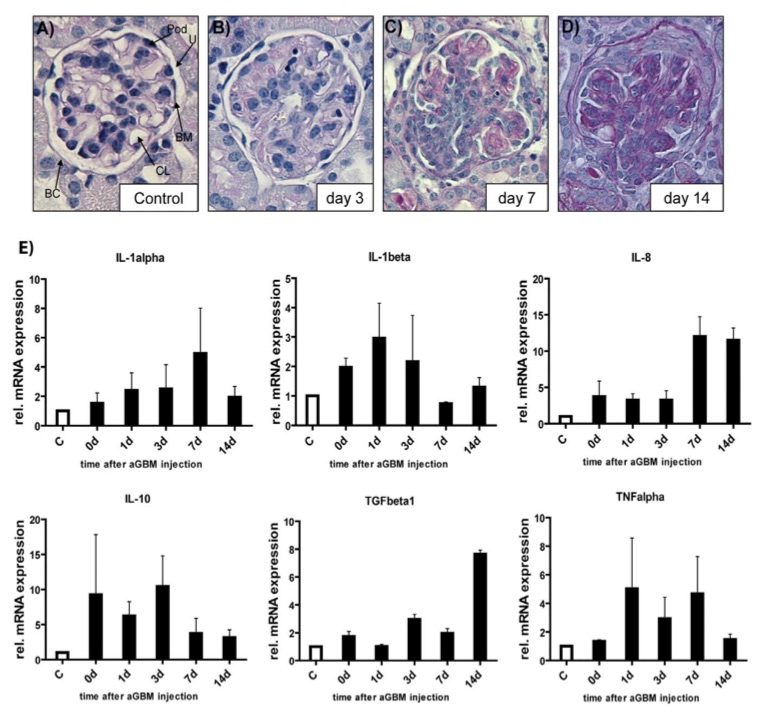 Fig.1 Functionality of the anti-GBM nephritis model and differential cytokine activation.1
Fig.1 Functionality of the anti-GBM nephritis model and differential cytokine activation.1
Histological analysis was conducted at multiple time points to assess the functionality of the anti-GBM nephritis model. As demonstrated in Fig. 1A–D, the administration of anti-GBM antibodies resulted in glomerular inflammation, crescent formation, and tubular damage throughout the disease progression. To investigate the molecular changes associated with the inflammatory response, the expression of pro-inflammatory cytokines (TNF-α, IL-1β, IL-8) and anti-inflammatory cytokines (IL-10, TGF-β1) was analyzed using quantitative real-time PCR (qPCR) (Fig. 1E). TNF-α and IL-1β mRNA levels were significantly elevated during the initial 7 days of the disease. In contrast, IL-8 expression was markedly increased in the later stages of the disease. Additionally, the counter-regulatory cytokine IL-10 was upregulated early in the disease process. Notably, TGF-β1 expression was significantly higher at the later stages of anti-GBM nephritis, potentially correlating with crescent formation observed during this phase of the disease.
Reference
- Müller, Ralf et al. "The mitogen-activated protein kinase p38α regulates tubular damage in murine anti-glomerular basement membrane nephritis." PloS one vol. 8,2 (2013): e56316. Distributed under an Open Access license CC BY 4.0, without modification. https://doi.org/10.1371/journal.pone.0056316
For Research Use Only.
