Femoral Artery Ligation induced Lower Limb Peripheral Vascular Disease Modeling & Pharmacodynamics Service
Introduction
Peripheral vascular disease (PVD) is a chronic circulatory condition where narrowed arteries reduce blood flow to the limbs, most commonly the legs. This can lead to pain, non-healing wounds, and in severe cases, amputation. Understanding PVD pathophysiology and developing effective therapies requires robust preclinical models.
Creative Biolabs is committed to advancing PVD research, offering a variety of well-established rodent models to evaluate the efficacy of novel therapeutic strategies accurately.
Femoral Artery Ligation-Induced PVD Model in Lower Limbs
The femoral artery ligation model is a widely recognized and indispensable preclinical tool for studying peripheral ischemia and evaluating therapeutic interventions aimed at improving blood flow and tissue viability. This model involves the surgical occlusion of the femoral artery in the lower limb of rodents, precisely mimicking an acute ischemic event and triggering the body's natural compensatory mechanisms, such as angiogenesis and arteriogenesis.
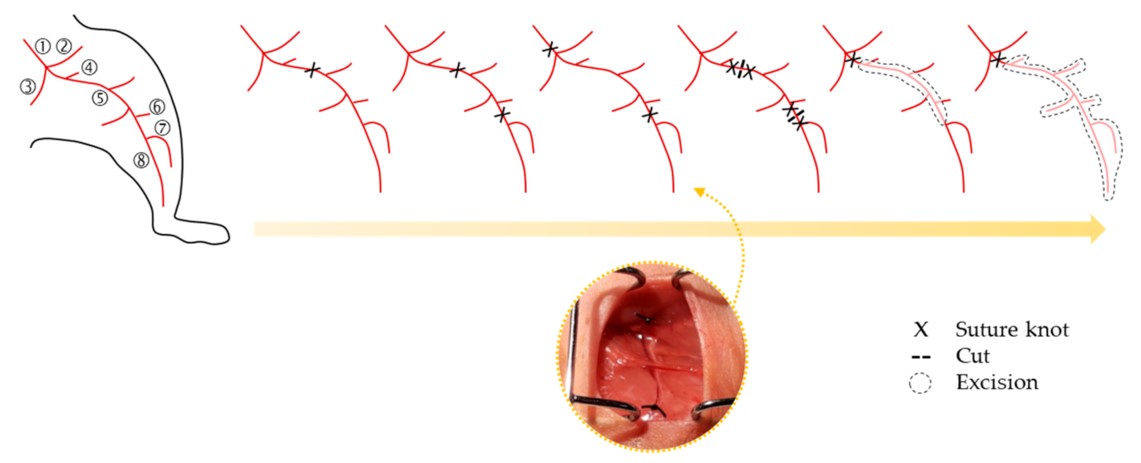 Fig.1 Schematic representation of femoral artery ligation strategies.1,3
Fig.1 Schematic representation of femoral artery ligation strategies.1,3
Model Construction Steps
The construction of the femoral artery ligation model is a precise surgical procedure designed to induce consistent and severe hind limb ischemia. This involves carefully isolating and ligating the common femoral artery in the experimental animal, typically a mouse or rat, to ensure a reproducible reduction in blood flow to the distal limb.
01Anesthesia and Preparation
Animals are anesthetized using appropriate agents and placed in a supine position. The surgical area (inner thigh) is shaved and disinfected.
02Incision and Exposure
A small incision is made along the inner thigh to expose the common femoral artery, vein, and nerve bundle. Care is taken to minimize damage to surrounding tissues.
03Artery Ligation
The common femoral artery is carefully separated from the femoral vein and nerve. It is then ligated (tied off) at two points, typically distal to the profunda femoris artery and proximal to its bifurcation into the superficial and saphenous arteries, using fine surgical sutures. This complete occlusion ensures severe ischemia.
04Muscle and Skin Closure
The overlying muscle layers are carefully reapproximated, and the skin incision is closed using surgical sutures or clips.
05Post-Operative Care
Animals receive analgesia and are monitored closely for recovery. Warmth is provided to prevent hypothermia, and hydration is ensured.
Strengths and Limitations
Strengths:
- High Reproducibility: Standardized surgical protocols and experienced technicians ensure consistent ischemic injury across experimental groups.
- Clinical Relevance: Accurately mimics acute limb ischemia and the subsequent processes of angiogenesis and arteriogenesis observed in human PVD.
- Detailed Pathophysiological Insights: Allows for a comprehensive study of muscle degeneration, nerve damage, and tissue remodeling responses to ischemia.
Limitations:
- Acute Ischemia Model: Primarily models acute occlusion rather than chronic, progressive atherosclerosis, which characterizes much of human PVD.
- Surgical Variability: Requires highly skilled surgical teams to minimize variability in ligation effectiveness and ensure consistent outcomes.
Evaluation Platform
Creative Biolabs provides a robust evaluation platform to comprehensively assess the efficacy of therapeutic interventions in the femoral artery ligation model. Our state-of-the-art facilities enable detailed biochemical, molecular, cellular, histopathological, behavioral, and imaging analyses, ensuring a holistic understanding of treatment effects.
Key Test Indicators:
- Limb Perfusion: Laser Doppler Perfusion Imaging (LDPI) for quantitative blood flow recovery.
- Functional Recovery: Gait analysis, limb salvage rates, toe necrosis scoring, and assessment of muscle contraction force via sciatic nerve stimulation.
- Histological Analysis: Quantification of capillary density (e.g., CD31 staining), muscle fiber size, necrosis, fibrosis, and adipose tissue accumulation.
- Molecular Analysis: Gene and protein expression of angiogenic factors (e.g., VEGF, HIF-1α), inflammatory markers (e.g., TNF-α, IL-6), and markers of oxidative stress.
- Neuromuscular Junction (NMJ) Integrity: Histological assessment of NMJ structure and density.
Applications
- Disease Modeling: This model serves as a robust platform for simulating critical limb ischemia (CLI), peripheral arterial disease (PAD), and acute limb ischemia, enabling researchers to study disease progression and therapeutic responses in a controlled in vivo environment.
- Therapeutic Efficacy Assessment: It is extensively utilized for evaluating a broad spectrum of therapeutic interventions, including pro-angiogenic drugs, anti-inflammatory agents, cell-based therapies, gene therapies, and novel biomaterials, all aimed at promoting revascularization, reducing tissue damage, and improving limb function.
- Mechanistic Research: Beyond therapeutic testing, the model is invaluable for elucidating the complex molecular and cellular mechanisms underlying ischemia-induced angiogenesis, muscle degeneration, nerve damage, and tissue repair processes in the context of peripheral vascular disease.
Related Peripheral Vascular Disease Models
Our Advantages
- Decades of Expertise: Years specializing in cardiovascular disease models, ensuring unparalleled scientific insight.
- Unrivaled Reproducibility: Strict adherence to standardized surgical protocols and rigorous quality control measures for consistent results.
- Comprehensive Phenotyping: Access to a full spectrum of advanced in vivo and ex vivo analytical techniques for deep insights.
- Tailored Study Designs: Flexible and customizable study protocols to precisely align with your unique research objectives and therapeutic candidates.
- Expert Scientific Consultation: Our seasoned biologists offer invaluable guidance from study design through data interpretation, maximizing your research impact.
Work with Us
- Summarize the project requirements and fill in the information collection form.
- Sign a CDA from both parties to further communicate information, such as targets.
- Select an animal model, discuss experimental design, and determine assay parameters.
- Project costing and project schedule forecasting.
- We provide a detailed project plan, including the required sample quantities, methods, and protocols.
- Both parties confirm the project details and start the project.
- Confirm the timeline of the project.
- We provide periodic results and information on the animal's condition.
- We will work together to make project adjustments as necessary.
- We provide a comprehensive project report promptly.
- We arrange transportation for the produced samples.
- We provide a discussion of the project results and help to arrange the next steps.
- Data storage and archiving.
Contact Us
Creative Biolabs is dedicated to providing high-quality preclinical research services that accelerate your therapeutic development. We offer meticulously executed models and comprehensive analytical support. We encourage you to contact us to discuss how our expertise can advance your specific research goals in peripheral vascular disease.
FAQs
-
Q1: Why is the femoral artery ligation model considered a gold standard for PVD research?
A: This model is highly valued because it accurately simulates the acute ischemic event seen in human peripheral vascular disease. It reliably triggers the body's natural processes of angiogenesis and arteriogenesis, allowing researchers to study how new blood vessels form and how existing ones remodel in response to reduced blood flow, which is crucial for developing effective therapies.
-
Q2: How do you ensure the reproducibility of the femoral artery ligation procedure?
A: We maintain stringent standardization of our surgical protocols, performed by highly experienced and specialized surgical teams. Our internal quality control measures include consistent ligation techniques, careful post-operative monitoring, and regular validation of ischemic induction through techniques like Laser Doppler Perfusion Imaging to ensure minimal variability across studies.
-
Q3: What specific functional assessments are performed to evaluate limb recovery in this model?
A: Beyond general observations like limb salvage and toe necrosis, we employ more objective functional assessments. These include quantitative gait analysis to measure walking ability and more advanced techniques such as evaluating skeletal muscle contraction force stimulated via the sciatic nerve, which provides direct insight into nerve and muscle integrity post-ischemia.
-
Q4: Do you provide support for interpreting the complex data generated from this model?
A: Absolutely. Our team of expert biologists, with extensive experience in cardiovascular research, provides comprehensive scientific consultation. We work closely with our clients to interpret the generated data, discuss its implications, and help strategize the next steps in your research, ensuring you derive maximum value from your study.
-
Q5: Can you integrate this model with other disease models or specific genetic backgrounds?
A: Yes, our customizable study design capabilities allow for significant flexibility. We can integrate the femoral artery ligation model with various genetic backgrounds (e.g., diabetic, hyperlipidemic mouse models) to investigate PVD in specific disease contexts. We also offer co-ligation or other modifications to create more complex or severe ischemic conditions as required by your research.
Published Data
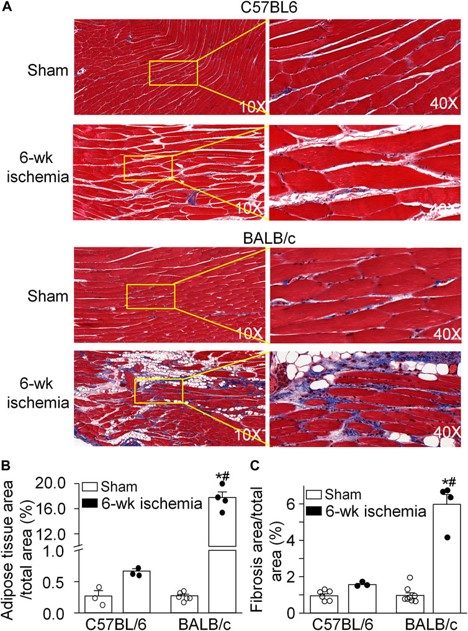 Fig.2 Pathological alterations of gastrocnemius muscles induced by the femoral artery ligation (ischemia).2,3
Fig.2 Pathological alterations of gastrocnemius muscles induced by the femoral artery ligation (ischemia).2,3
This study involves the use of the femoral artery ligation-induced PVD model in mice to investigate strain-specific skeletal muscle responses to ischemia. Researchers compared the morphological and functional alterations in the gastrocnemius muscle of BALB/c and C57BL/6 mice after femoral artery ligation. The project successfully revealed that BALB/c mice exhibited more severe muscular dystrophy, increased adipose tissue accumulation, and greater fibrosis, along with more pronounced damage to neuromuscular junctions and weakened muscle contraction, compared to C57BL/6 mice. This highlights the importance of genetic background in PVD modeling and demonstrates how the models can identify optimal strains for developing new therapeutic approaches to improve limb structure and function.
References
- Beltrán-Camacho, Lucía et al. "Current Status of Angiogenic Cell Therapy and Related Strategies Applied in Critical Limb Ischemia." International journal of molecular sciences vol. 22,5 2335. 26 Feb. 2021. https://doi.org/10.3390/ijms22052335
- Tu, Huiyin et al. "Different responses of skeletal muscles to femoral artery ligation-induced ischemia identified in BABL/c and C57BL/6 mice." Frontiers in physiology vol. 13 1014744. 16 Sep. 2022. https://doi.org/10.3389/fphys.2022.1014744
- Distributed under Open Access license CC BY 4.0, without modification.
For Research Use Only.
