Pulmonary Artery (PA) Constriction induced Right Heart Failure Modeling & Pharmacodynamics Service
At Creative Biolabs, we recognize the urgent need for innovative solutions in this field. Our extensive expertise allows us to provide a diverse range of meticulously characterized, well-established in vivo models, designed to effectively evaluate the efficacy of promising HF therapeutics.
Introduction
Heart failure (HF) represents a profoundly life-threatening and debilitating syndrome, characterized by the heart's diminished capacity to effectively pump blood or adequately fill its chambers. This pervasive condition impacts a staggering number of individuals, with over 64 million people affected globally. Its complex nature, encompassing diverse etiologies and progressing through various stages, ultimately leads to substantial morbidity, significant reductions in quality of life, and premature mortality.
Pulmonary Artery (PA) Constriction-Induced Right HF Model
The pulmonary artery (PA) constriction-induced right heart failure (RHF) model is a cornerstone in preclinical cardiovascular research, specifically designed to investigate pressure overload-induced RHF independently of primary pulmonary vascular changes. This model is critical for understanding the myocardial response to chronic afterload.
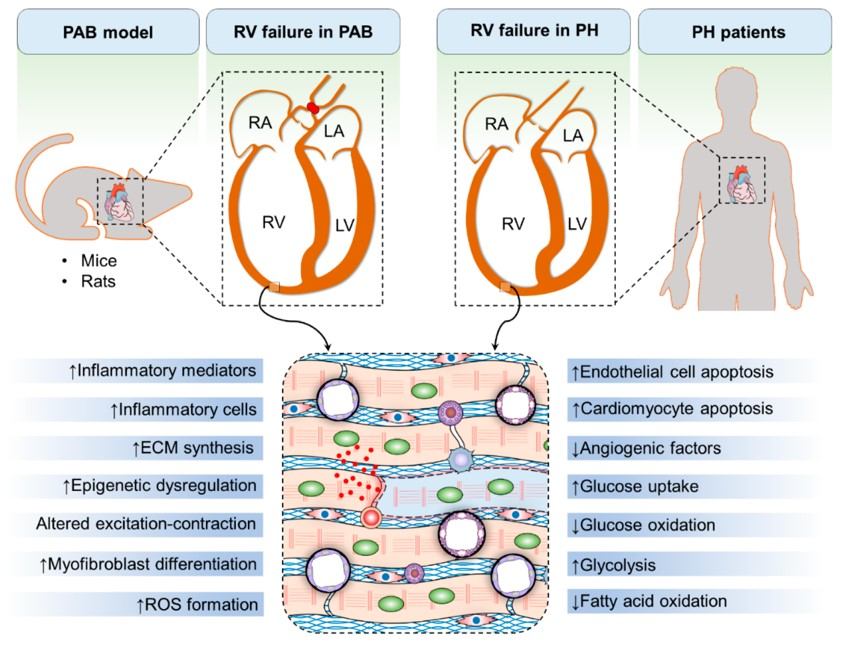 Fig.1 Features of RHF reproduced by the pulmonary artery banding (PAB) RHF model.1,3
Fig.1 Features of RHF reproduced by the pulmonary artery banding (PAB) RHF model.1,3
Model Construction Steps
The construction of the PA constriction model involves a precise surgical procedure in rodents, typically rats or mice:
01Preparation
Animals are anesthetized, and appropriate surgical fields are prepared with aseptic techniques.
02Thoracotomy
A left thoracotomy is performed, providing access to the thoracic cavity and the heart.
03Pulmonary Artery Exposure
The main pulmonary artery (mPA) is carefully isolated and exposed.
04Band Placement
A constrictive band (often a small clip or a suture tied around a needle of a specific gauge, which is then removed) is meticulously placed around the mPA. This creates a fixed, sustained increase in pulmonary vascular resistance.
05Closure
The chest cavity is closed in layers, and the animal is allowed to recover.
Following banding, the right ventricle undergoes a well-defined progression: initial compensatory hypertrophy, followed by maladaptive remodeling (characterized by fibrosis, cardiomyocyte disarray, and metabolic shifts), and culminating in RV dysfunction and failure. Cardiac remodeling is meticulously monitored at specific timepoints using a combination of techniques to track disease progression.
Strengths and Limitations
Strengths:
- Clinical Relevance: Accurately mimics human pressure overload-induced RHF, including key pathological features like RV hypertrophy, fibrosis, and functional decline.
- Reproducibility: Offers consistent and reliable RV pressure overload and RHF development, minimizing experimental variability when performed by skilled researchers.
- Defined Progression: Allows for precise timing of therapeutic interventions at distinct disease stages.
- Isolated RV Focus: Enables the study of RV remodeling and failure independent of primary pulmonary vascular changes.
Limitations:
- Surgical Complexity: Requires precise surgical technique to ensure consistent banding and minimize complications.
- Species-Specific Nuances: While broadly applicable, there can be subtle differences in RV response and assessment challenges (e.g., echocardiography in awake mice) between rodent species.
Evaluation Platform
Creative Biolabs provides an advanced evaluation platform, deploying a wide array of investigative techniques to thoroughly characterize the PA Constriction-Induced RHF model and assess therapeutic efficacy.
Our capabilities include:
- Biochemical & Molecular Analysis: Assessment of gene expression (e.g., qPCR, RNA-Seq), protein levels (e.g., Western blot, ELISA), and critical signaling pathways, including metabolic dysregulation.
- Cellular Analysis: Histopathological examination for cardiomyocyte hypertrophy, fibrosis (Sirius Red), and inflammatory infiltrates.
- Histopathological & Gross Morphological Assessment: Careful dissection of the heart for precise RV hypertrophy measurement and histological sectioning for detailed microscopic analysis.
-
Physiological & Imaging Studies:
- Hemodynamic Measurements: Invasive right heart catheterization, typically via the internal jugular vein, directly assesses RV systolic and pulmonary artery pressures, cardiac output, and provides comprehensive live pressure-volume loops.
- Echocardiography: Non-invasive evaluation of RV dimensions, wall thickness, and functional parameters (e.g., FAC, TAPSE). Key indicators like tricuspid regurgitation Pulse Doppler and lateral tricuspid annulus Tissue Doppler, correlated with human PH mortality, are analyzed. Assessments are typically at 24 hours and 3 weeks post-PAB
Applications
- Disease Simulation: Faithfully simulates pressure overload-induced RHF, a common consequence of pulmonary hypertension (PAH) and other conditions leading to increased RV afterload. It reflects the obstructive pulmonary vasculopathy of PAH, characterized by vascular remodeling, inflammation, and vasoconstriction.
- Drug Evaluation: Ideal for screening novel therapeutic agents, including small molecules, biologics, and gene therapies, designed to prevent, halt, or reverse RV dysfunction.
- Treatment Strategies: Used to investigate two primary therapeutic approaches: those targeting pulmonary vascular resistance to reduce RV afterload, and those directly improving RV adaptation and function. The model also allows for the assessment of drug combinations and the validation of new biomarkers for disease progression and therapeutic response.
Related Heart Failure Models
Ascending Aortic Arch Constriction induced Post-Pressure Overload Heart Failure Model
Abdominal Aortic Stenosis induced Left HF Model
DOCA & Salt induced Left HF Model
Adriamycin induced Left HF Model
Our Advantages
- Unrivaled Scientific Acumen: Our team possesses deep biological knowledge crucial for complex disease models.
- Precision and Reproducibility: Meticulous surgical techniques ensure consistent model induction and reliable data.
- Comprehensive Phenotyping: We offer a full spectrum of advanced analytical techniques for thorough assessment.
- Translational Focus: Our models and analyses are designed to yield data highly relevant to human disease.
- Seamless Regulatory Support: We provide data for preclinical efficacy, supporting your IND filings and regulatory journey.
- Customized Study Design: Protocols are tailored precisely to meet your unique research objectives.
Work with Us
- Summarize the project requirements and fill in the information collection form.
- Sign a CDA from both parties to further communicate information, such as targets.
- Select an animal model, discuss experimental design, and determine assay parameters.
- Project costing and project schedule forecasting.
- We provide a detailed project plan, including the required sample quantities, methods, and protocols.
- Both parties confirm the project details and start the project.
- Confirm the timeline of the project.
- We provide periodic results and information on the animal's condition.
- We will work together to make project adjustments as necessary.
- We provide a comprehensive project report promptly.
- We arrange transportation for the produced samples.
- We provide a discussion of the project results and help to arrange the next steps.
- Data storage and archiving.
Contact Us
Connect us today to explore how our expertise in the pulmonary artery constriction-induced RHF model can be instrumental in achieving your next therapeutic breakthrough. We are eager to discuss your specific project needs.
FAQs
-
Q1: What are the primary advantages of using the Pulmonary Artery Constriction (PAC) model over other HF models for studying RHF?
A: The PAC model uniquely provides a clear focus on the right ventricle's response to chronic pressure overload, separate from primary pulmonary vascular changes. This fixed afterload condition allows for precise investigation of myocardial remodeling and dysfunction, which is often difficult to isolate in other systemic HF models. Its high reproducibility and well-characterized disease progression are also significant benefits for robust preclinical studies.
-
Q2: What specific timepoints do you recommend for assessing cardiac remodeling and function post-PA banding, and why?
A: While study designs are customized, we typically recommend initial non-invasive echocardiography at 24 hours post-PAB to confirm successful banding, followed by comprehensive assessments around 3 weeks. The 3-week mark is often critical as it captures the transition from compensatory hypertrophy to early maladaptive remodeling, allowing for evaluation of interventions aimed at preventing failure. Further timepoints are chosen based on the desired stage of RHF and therapeutic goals.
-
Q3: Can this model be used to differentiate between therapies that reduce RV afterload and those that directly improve RV myocardial function?
A: Absolutely. The PA Constriction model, by imposing a fixed afterload, is uniquely suited to evaluate interventions targeting the RV myocardium directly. When combined with comprehensive hemodynamic assessments, it allows researchers to dissect whether a therapeutic agent is primarily reducing pulmonary vascular resistance (less relevant in this fixed-afterload model, unless the intervention is designed to do so directly) or specifically improving the RV's intrinsic contractile or adaptive capabilities.
-
Q4: Is the PA Constriction model suitable for long-term studies, and what considerations are important for such designs?
A: Yes, the model can be adapted for long-term studies to observe progressive RHF and chronic therapeutic effects. For extended durations, considerations include managing animal welfare, potential for variable compensatory responses over time, and the choice of appropriate endpoints that reflect late-stage disease. Regular non-invasive monitoring helps track progression without repeated invasive procedures.
-
Q5: Can Creative Biolabs help with customized study designs if our therapeutic agent targets a specific pathway or stage of RHF?
A: Absolutely. Customization is a core strength at Creative Biolabs. We collaborate closely with clients to tailor study designs, including specific dosing regimens, intervention timings (e.g., prevention vs. treatment of established RHF), and selection of targeted endpoints. Our scientific team provides expert consultation to ensure the experimental design precisely addresses your unique research questions.
Published Data
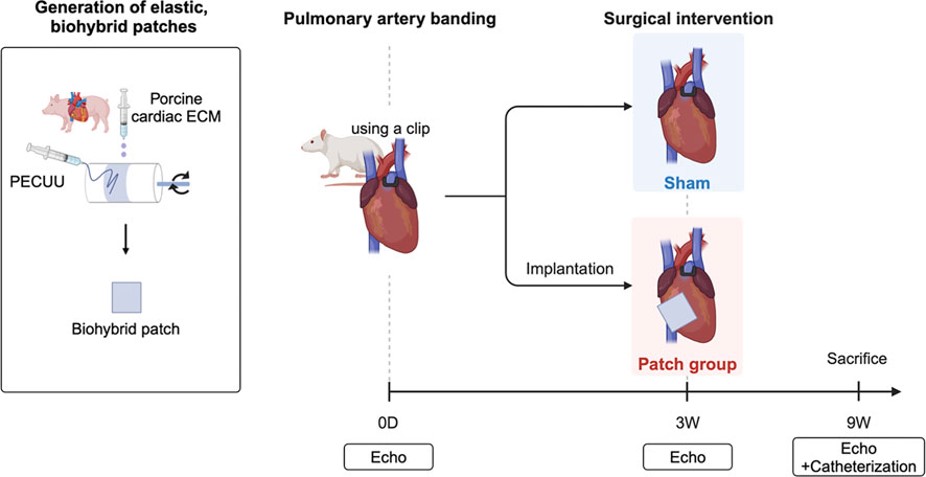 Fig.2 Construction of the model of RHF with PAB and patch placement.2,3
Fig.2 Construction of the model of RHF with PAB and patch placement.2,3
In a representative study, a team investigated the impact of placing a degradable, biohybrid patch onto the right ventricle in a rat model of RHF induced by PAB. Three weeks post-PAB, patches comprising poly (ester carbonate urethane) urea and porcine cardiac extracellular matrix were attached to the RV epicardium. Nine weeks later, a comprehensive evaluation revealed significant RV wall thickening and cavity enlargement, along with increased interstitial fibrosis in control animals. However, the patch group demonstrated improved myocardial output, moderated pressure stress, and notably reduced RV fibrosis, alongside improved left ventricular ejection fraction and tricuspid annular plane systolic excursion. This project highlights the model's utility in evaluating novel cardiac interventions aimed at improving RV function and reversing remodeling.
References
- Mamazhakypov, Argen et al. "Novel Therapeutic Targets for the Treatment of Right Ventricular Remodeling: Insights from the Pulmonary Artery Banding Model." International journal of environmental research and public health vol. 18,16 8297. 5 Aug. 2021. https://doi.org/10.3390/ijerph18168297
- Hayashi, Yasunari et al. "Placement of an elastic, biohybrid patch in a model of right heart failure with pulmonary artery banding." Frontiers in bioengineering and biotechnology vol. 12 1485740. 20 Jan. 2025. https://doi.org/10.3389/fbioe.2024.1485740
- Distributed under Open Access license CC BY 4.0, without modification.
For Research Use Only.
