Diet induced Obesity (DIO) Non-Alcoholic Steatohepatitis (NASH) Modeling & Pharmacodynamics Service
Creative Biolabs offers a wide range of animal models to evaluate the efficacy of NASH treatments, ensuring tailored solutions to meet your specific research needs. We specialize in providing accurate and reliable models for drug development, from early-stage screening to advanced therapeutic trials.
Introduction
Non-alcoholic steatohepatitis (NASH) is a progressive liver disease that is part of the spectrum of non-alcoholic fatty liver disease (NAFLD). NASH is characterized by liver inflammation, fat accumulation, and liver cell injury, which can eventually lead to fibrosis, cirrhosis, and even hepatocellular carcinoma (HCC). It is strongly associated with metabolic disorders, such as obesity, insulin resistance, type 2 diabetes, and hyperlipidemia. The disease is becoming increasingly prevalent worldwide due to rising obesity rates and poor dietary habits. In the early stages, NASH may not exhibit noticeable symptoms, but over time, it can cause significant liver damage. Risk factors for NASH include metabolic syndrome, dyslipidemia, and genetic predisposition. Diagnosis is typically made through liver biopsy or imaging studies, with liver enzymes (ALT, AST) often elevated in blood tests. There is currently no FDA-approved pharmacological treatment for NASH, and management focuses on lifestyle changes, including weight loss, dietary modifications, and managing comorbidities. However, numerous therapeutic agents are under investigation to halt or reverse the progression of the disease.
Disease Models and Applications
The Diet induced Obesity (DIO) NASH model is an established method for inducing NASH in rodents by feeding them a high-fat diet (HFD) that leads to obesity and metabolic abnormalities like those observed in humans. The model effectively mimics the progression of NAFLD to NASH, offering a reliable system for studying the pathogenesis and evaluating potential treatments. To induce NASH, rodents are fed a high-fat, high-calorie diet for extended periods, typically between 8-12 weeks. This diet leads to liver fat accumulation, insulin resistance, and inflammation, which are key features of NASH. One of the advantages of this model is its simplicity and the ability to induce obesity-related liver disease in a relatively short period. However, it does not always replicate the genetic aspects of human NASH, making it less suitable for studying genetic predispositions to the disease.
- Simulates: The DIO NASH model simulates non-alcoholic fatty liver disease progression to NASH, including the development of liver steatosis, inflammation, and fibrosis commonly observed in human patients with metabolic syndrome.
- Evaluates Drugs: This model is used to evaluate the efficacy of various therapeutic interventions, such as statins, PPAR agonists, FXR agonists, and other anti-inflammatory or anti-fibrotic drugs. It helps in assessing the impact of treatments on liver fat accumulation, inflammatory markers, fibrosis progression, and overall liver function.
Measurements
We offer a variety of measurements for evaluating drug efficacy in the Diet induced Obesity (DIO) NASH Model, utilizing advanced techniques, including but not limited to:
- General observations: Body weight, food intake, mortality rate, and physical activity levels.
- Liver function tests: Serum levels of liver enzymes (ALT, AST), bilirubin levels, and hepatic triglyceride content.
- Histopathological analysis: Liver tissue examination for steatosis, inflammation, hepatocyte ballooning, and fibrosis, using Hematoxylin and Eosin (H&E) and Masson's Trichrome staining.
- Cytokine profiling (e.g., ELISA): Measurement of inflammatory cytokines such as TNF-α, IL-6, and IL-1β.
- Gene/protein expression analysis: RT qPCR and Western blot to assess expression of key genes and proteins involved in lipid metabolism, inflammation, and fibrosis (e.g., PPARγ, TNF-α, collagen type I).
- Immunohistochemistry: Infiltration of immune cells (e.g., macrophages, T-cells) in liver tissue.
In addition to the DIO NASH model, we can develop custom animal models based on literature and specific research needs to meet your project objectives. Our scientific team is available to assist with experimental design, model selection, and data analysis, ensuring your project's success.
Related Services
In addition to the DIO NASH model, we offer several other methods for inducing NASH. These models allow for a broader investigation of NASH pathogenesis and therapeutic development under various metabolic conditions.
- High-Fat Diet induced NASH Model
- Methionine Choline-Deficient (MCD) Diet induced NASH Model
- Choline-Deficient L-Amino Acid-Defined (CDAA) Diet induced NASH Model
- High-Fat & High-Carbohydrate Diet induced NASH Model
- High-Fat & High-Cholesterol Diet induced NASH Model
- High-Fat & High-Cholesterol Diet & Fructose induced NASH Model
- High-Fat & Fructose induced NASH Model
- Diethylnitrosamine (DEN) & High-Fat & High-Carbohydrate Diet induced NASH Model
- High-Fat & CCL4 induced NASH Model
- Streptozotocin (STZ) & High-Fat induced NASH Model
- MC4R KO Mouse Model
- LDLR KO Mouse Model
Advantages
- Customization: We offer flexible and tailored approaches to model development based on the specific requirements of your research.
- Comprehensive services: From model creation to data analysis, we provide end-to-end support to ensure the success of your study.
- State-of-the-art technologies: We use cutting-edge techniques, such as gene expression profiling, advanced imaging, and immunohistochemistry, to deliver high-quality results.
- Collaboration: Our dedicated team works closely with you, offering expert advice on experimental design, model selection, and data interpretation.
- Reliable and reproducible results: We adhere to strict quality control protocols, ensuring that the results from our models are consistent and reproducible across studies.
Work with Us
- Summarize the project requirements and fill in the information collection form.
- Sign a CDA from both parties to further communicate information, such as targets.
- Select an animal model, discuss experimental design, and determine assay parameters.
- Project costing and project schedule forecasting.
- We provide a detailed project plan, including the required sample quantities, methods, and protocols.
- Both parties confirm the project details and start the project.
- Confirm the timeline of the project.
- We provide periodic results and information on the animal's condition.
- We will work together to make project adjustments as necessary.
- We provide a comprehensive project report promptly.
- We arrange transportation for the produced samples.
- We provide a discussion of the project results and help to arrange the next steps.
- Data storage and archiving.
FAQs
-
Q: How is the Diet induced Obesity (DIO) NASH Model created?
A: The DIO NASH model is induced by feeding rodents a high-fat diet to promote obesity and the progression of fatty liver disease to NASH.
-
Q: What types of drugs can be evaluated in the DIO NASH model?
A: Drugs such as statins, PPAR agonists, FXR agonists, and anti-inflammatory or anti-fibrotic agents can be tested for their effects on liver function, inflammation, and fibrosis in this model.
-
Q: What measurements are used to assess drug efficacy in this model?
A: Measurements include liver enzyme levels, histopathological analysis, cytokine profiling, and gene/protein expression related to lipid metabolism and fibrosis.
-
Q: Can you develop custom NASH models for specific research needs?
A: Yes, we offer customized NASH models based on specific study requirements and can help in experimental design and data analysis for your unique research goals.
Published Data
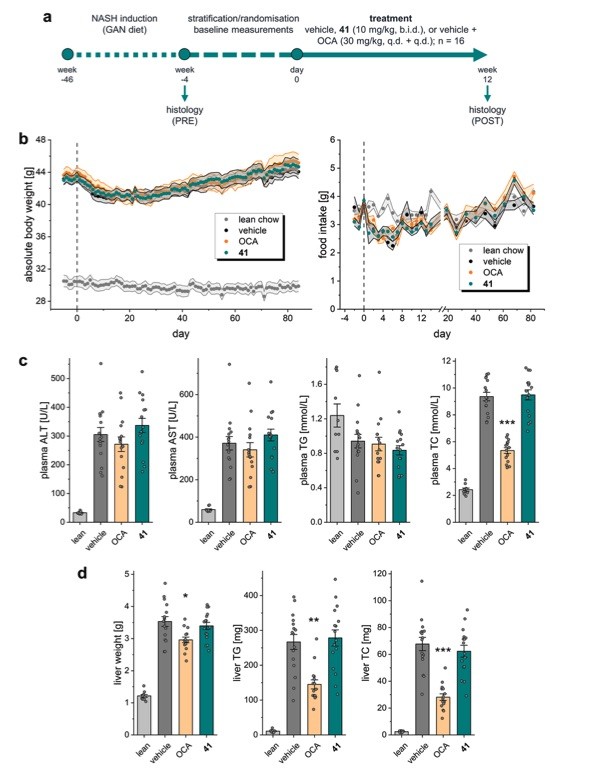 Fig. 1 Characterization of 41 in diet-induced obese (DIO) NASH in mice.1
Fig. 1 Characterization of 41 in diet-induced obese (DIO) NASH in mice.1
This article evaluated the efficacy of compound 41, a triple FXR/PPARα/δ modulator, using the diet induced obesity (DIO) non-alcoholic steatohepatitis (NASH) model in mice. This model was chosen for its high reliability in mimicking human NASH and has previously been used to assess the effects of combined OCA/elafibranor treatment. NASH was induced in 48 mice (16 per group) over a 46-week period with a specialized diet containing 40% fat (primarily palm oil), 40% carbohydrates (20% fructose), and 2% cholesterol (Gubra AMLN NASH diet). After confirming the presence of NASH via biopsy, the mice were treated with 41 (10 mg/kg, b.i.d.), OCA (30 mg/kg), or vehicle, while maintaining the NASH-inducing diet for 12 weeks. Throughout the treatment phase, all animals exhibited normal behavior with no significant differences in food intake or body weight between the groups. However, one mouse in the OCA group died during the second week of treatment. At the four-week mark, no significant changes were observed in biochemical parameters between the groups, except for reduced total cholesterol (TC) levels in the OCA group. After 12 weeks, plasma levels of liver enzymes (ALT, AST) and triglycerides (TG) showed no significant differences between the groups. While OCA treatment reduced hepatic fat content and steatosis, compound 41 did not show pronounced effects on steatosis or liver weight, triglyceride, or cholesterol levels. These findings suggest that while 41 demonstrated potential in in vitro and pilot in vivo profiling, it did not significantly improve the NASH-related biomarkers in this model.
Reference
- Heitel, Pascal et al. "A triple farnesoid X receptor and peroxisome proliferator-activated receptor α/δ activator reverses hepatic fibrosis in diet induced NASH in mice." Communications chemistry vol. 3,1 174. 13 Nov. 2020, DOI:10.1038/s42004-020-00411-z. Distributed under an Open Access license CC BY 4.0, without modification.
For Research Use Only.
