- Summarize the project requirements and fill in the information collection form.
- Sign a CDA from both parties to further communicate information, such as targets.
- Select an animal model, discuss experimental design, and determine assay parameters.
- Project costing and project schedule forecasting.
Permanent Ischemic Myocardial Infarction Modeling & Pharmacodynamics Service
Creative Biolabs, with over decades of leadership in preclinical research, provides a diverse range of meticulously validated models, empowering researchers to comprehensively evaluate potential interventions against MI.
Introduction
Myocardial Infarction (MI), commonly known as a heart attack, represents a critical health burden globally, leading to significant morbidity and mortality. Beyond the acute event, its long-term consequences, particularly the progression to chronic heart failure through adverse ventricular remodeling, pose immense challenges. To effectively combat this, a profound understanding of the complex biological processes initiated by sustained ischemia and the development of innovative therapies to mitigate myocardial damage are crucial.
Permanent Ischemic Myocardial Infarction Model
The permanent ischemic MI model is a cornerstone in cardiovascular research, meticulously designed to replicate the pathological events following an irreversible coronary artery occlusion, mirroring severe human heart attack scenarios. This model is predominantly established through the permanent surgical ligation of the left anterior descending (LAD) coronary artery in various species (Mouse, Rat, Rabbit, Dog, NHPs), offering a highly reproducible platform for studying chronic cardiac remodeling and evaluating long-term therapeutic effects.
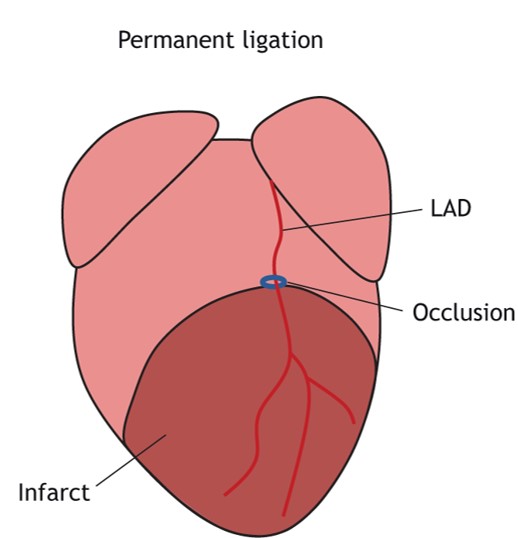 Fig.1 The infarcts generated after permanent ischemic techniques.1
Fig.1 The infarcts generated after permanent ischemic techniques.1
Model Construction Steps
The construction of this model involves a precise surgical strategy to ensure consistent infarct size and minimized post-operative complications.
Animals (Mouse, Rat, Rabbit, Dog, NHPs) are first anesthetized with inhaled agents, followed by careful intubation without tracheotomy to facilitate mechanical-assisted ventilation. Positive end-expiratory pressure is applied to maintain lung function.
A sparsely invasive left-sided thoracotomy is performed, carefully limiting surgical lesions to expose theheart. Ribs are gently retracted to reveal the left ventricle.
The left anterior descending coronary artery is identified, typically appearing as a prominent vessel running from the left auricle towards the apex. An irreversible ligation is then made with a fine suture, approximately 2-3 mm distal to its origin. Immediate blanching of the lower left ventricle confirms successful occlusion.
After ligation, the heart is carefully returned to the chest cavity. The chest wall and skin incisions are meticulously closed, often with a 22G catheter needle inserted to remove excess air and restore negative intrathoracic pressure, avoiding thoracentesis. Post-operative care includes continuous monitoring, warmth, and analgesia to ensure animal welfare and optimal recovery.
Advantages and Considerations
Advantages:
- Reproducibility: The standardized surgical technique yields highly consistent infarct sizes, crucial for reliable comparative studies.
- Chronic Disease Progression: Ideal for investigating chronic maladaptive ventricular remodeling, fibrosis, and functional decline over extended periods, reflecting the natural history of human chronic ischemic heart disease.
- Translational Relevance: The pathological cascade closely mirrors severe, persistent ischemic events in humans, providing a robust platform for preclinical drug development.
Considerations:
- This highly reproducible model demands significant technical expertise and specialized animal care. Creative Biolabs' experienced surgical teams and meticulous protocols are specifically designed to manage these complexities, ensuring consistent outcomes and minimizing variability.
Evaluation Platform
Creative Biolabs provides a comprehensive suite of evaluation platforms to thoroughly assess therapeutic efficacy within the permanent ischemic MI model. Our state-of-the-art facilities enable multi-dimensional analysis across various biological levels:
Key Test Indicators:
Imaging: Advanced echocardiography and MRI for non-invasive assessment of cardiac structure and function.
Indicators: Left ventricular ejection fraction (LVEF), fractional shortening (LVFS), end-diastolic and end-systolic volumes (LVEDV, LVESV), wall motion abnormalities, myocardial strain.
Hemodynamics: Invasive pressure-volume loop analysis for precise functional measurements.
Indicators: Left ventricular end-diastolic pressure (LVEDP), maximum pressure rise/fall (±dP/dtmax), stroke volume, cardiac output.
Histopathology: Tissue staining and microscopy for morphological changes.
Indicators: Infarct size, myocardial fibrosis (collagen content), cardiomyocyte hypertrophy, capillary density, inflammatory cell infiltration.
Biochemical & Molecular Analysis: Assessment of circulating biomarkers and tissue-level expression.
Indicators: Cardiac enzymes (Troponin I/T), inflammatory cytokines, oxidative stress markers, gene and protein expression related to hypertrophy, fibrosis, and apoptosis.
Cellular Analysis: Immunohistochemistry and flow cytometry for cell-specific responses.
Indicators: Proliferation, apoptosis, immune cell phenotyping, progenitor cell mobilization.
Applications
Simulated Diseases: Primarily used to mimic and study chronic ischemic heart disease, post-MI heart failure, and adverse ventricular remodeling. It effectively replicates the long-term consequences of a sustained coronary occlusion, providing insights into progressive cardiac dysfunction.
Drug Evaluation: Ideal for assessing the efficacy of novel compounds, biologics, and cellular therapies targeting myocardial preservation and repair. This includes:
- Cardioprotective agents designed to limit initial ischemic injury.
- Anti-remodeling therapies aimed at halting or reversing pathological ventricular changes.
- Regenerative medicine strategies focusing on myocardial repair and functional restoration, such as stem cell therapies or gene therapies.
Biomarker Discovery: Serves as a robust platform for identifying and validating novel diagnostic and prognostic biomarkers for MI progression and therapeutic response.
Related Myocardial Infarction Models
Our Advantages
- Decades of Expertise: Years dedicated to cardiovascular models.
- Precision and Reproducibility: Meticulous surgical techniques ensure consistent, reliable data.
- Holistic Phenotyping: Advanced platforms for comprehensive functional and structural assessment.
- Stringent Quality Control: Adherence to rigorous standards for data integrity.
- Expert Data Interpretation: Experienced biologists and statisticians for actionable insights.
- Efficient Project Management: Timely delivery of high-quality data to accelerate your pipeline.
Work with Us
Inquiry Stage
Project Start
- We provide a detailed project plan, including the required sample quantities, methods and protocols.
- Both parties confirm the project details and start the project.
- Confirm the timeline of the project.
Project Progress
- We provide periodic results and information on the animal's condition.
- We will work together to make project adjustments as necessary.
Project Completion
- We provide a comprehensive project report promptly.
- We arrange transportation for the produced samples.
- We provide a discussion of the project results and help to arrange the next steps.
After-Sales Support
- Data storage and archiving.
Contact Us
Accelerate your therapeutic development pipeline with Creative Biolabs' permanent ischemic MI Model. Contact us and partner with our experienced team to gain robust, translatable data and make significant strides in combating cardiovascular disease.
FAQs
-
Q1: What animal species are typically used for the permanent ischemic MI model at Creative Biolabs?
A: Our permanent ischemic myocardial infarction models include a variety of species, including mice, rats, rabbits, dogs, and non-human primates (NHPs). Mice and rats are particularly well-suited for this purpose. These models offer significant advantages in genetic accessibility, cost-effectiveness, and established experimental protocols, making them ideal for high-throughput screening and detailed mechanistic studies.
-
Q2: How do you ensure the consistency of infarct size in the permanent ischemic MI model?
A: Infarct size consistency is paramount for reliable data. We achieve this through highly standardized surgical protocols, including precise LAD ligation techniques, experienced surgical teams, and meticulous post-operative monitoring. Our established procedures minimize variability, ensuring each animal exhibits a comparable ischemic insult.
-
Q3: Can you customize the permanent ischemic MI model for specific genetic backgrounds or co-morbidities?
A: Absolutely. We understand that research objectives can be highly specific. Our expertise allows for customization of the model to incorporate various genetic backgrounds of animals or to introduce relevant co-morbidities, such as hypertension or diabetes, to better reflect complex human pathological conditions.
-
Q4: What are the primary endpoints measured to evaluate therapeutic efficacy in this model?
A: We employ a comprehensive suite of endpoints to assess therapeutic effects. These include non-invasive cardiac imaging (echocardiography, MRI) for functional parameters like ejection fraction and chamber dimensions, invasive hemodynamics for contractility, histological analyses for infarct size and fibrosis, and molecular assays for gene and protein expression related to cardiac remodeling.
-
Q5: Do you provide support for data analysis and scientific interpretation of the results?
A: Yes, beyond generating high-quality data, we offer extensive support in data analysis. Our team of experienced biologists and biostatisticians works collaboratively with clients to interpret findings, identify key trends, and provide insightful scientific conclusions, helping to accelerate decision-making in your research.
Published Data
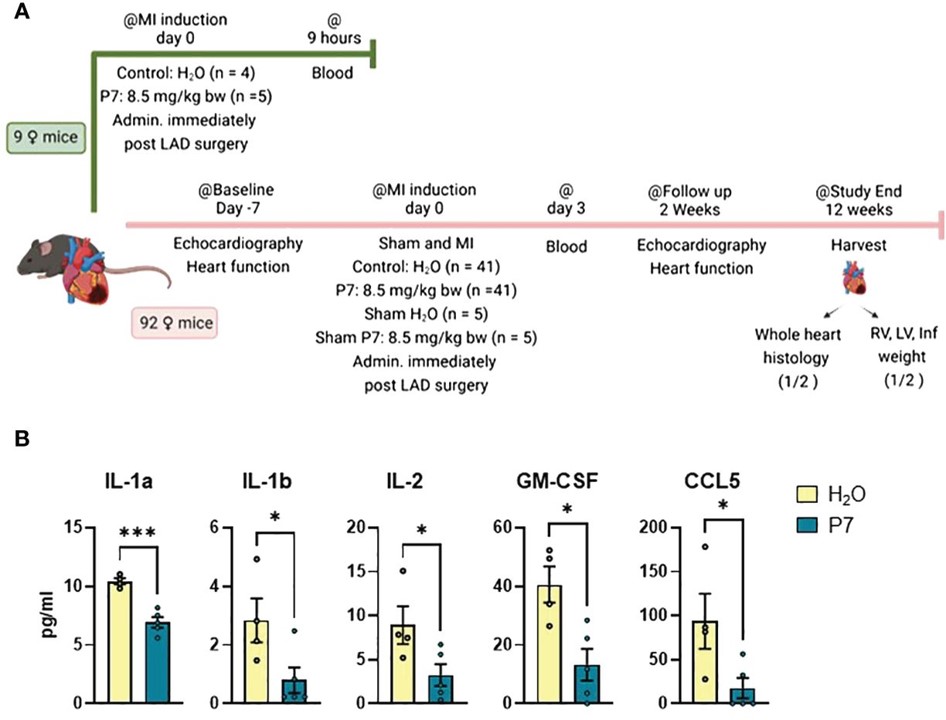 Fig.2 Study on myocardial inflammation post-MI using permanent ischemic MI model.2
Fig.2 Study on myocardial inflammation post-MI using permanent ischemic MI model.2
The permanent ischemic MI model is supported by extensive research and published findings, demonstrating its utility in understanding cardiac injury and repair. This research explored the beneficial effect of immediately administering a specific peptide (P7) post-permanent LAD ligation in mice. The results indicated that P7 administration initially dampened the secretion of inflammatory cytokines, and echocardiography revealed less deterioration of cardiac contraction in treated mice. This work exemplifies the model's application in evaluating novel cardioprotective agents and understanding the early inflammatory responses after MI.
References
- De Villiers, Carla, and Paul R Riley. "Mouse models of myocardial infarction: comparing permanent ligation and ischaemia-reperfusion." Disease models & mechanisms vol. 13,11 dmm046565. 18 Nov. 2020, DOI:10.1242/dmm.046565. Distributed under Open Access license CC BY 4.0, without modification. The image was modified by extracting and using only part of the original image.
- Olsen, Maria Belland et al. "SLAMF1-derived peptide exhibits cardio protection after permanent left anterior descending artery ligation in mice." Frontiers in immunology vol. 15 1383505. 15 Apr. 2024, DOI:10.3389/fimmu.2024.1383505. Distributed under Open Access license CC BY 4.0, without modification.
For Research Use Only.
