Glaucoma Modeling & Pharmacodynamics Services
Introduction
Glaucoma is a widespread retinal neurodegenerative disease. It is considered the leading cause of irreversible blindness worldwide. Its pathogenesis is still being explored, and it has been confirmed that it is associated with increased intraocular pressure, gradual loss of retinal ganglion cells, and subsequent optic nerve damage. The exploration into the complex sequence of glaucomatous injury and the formulation of effective treatment strategies fundamentally rely on the strategic application of suitable animal models. Of particular note, research frequently engages murine, rabbit, and non-human primate models as pivotal tools in advancing this essential scientific inquiry. In capturing the essence of this affliction, a nuanced appreciation of these models can perhaps offer profound insights into both the aetiology and prospective therapeutic avenues for managing glaucoma. Creative Biolabs has constructed a variety of animal models to simulate the occurrence and development of human glaucoma to promote the development and evaluation of drugs to treat the disease.
Glaucoma Disease Models Available at Creative Biolabs
- NMDA-Induced Retinal Ganglion Cells (RGCs) Injury Models
N-methyl-D-aspartic acid (NMDA), an amino acid derivative acting as an excitatory neurotransmitter, plays a crucial role in neuronal signaling. Activation of NMDA receptors induces an influx of calcium ions within retinal ganglion cells (RGCs), precipitating cellular demise. Following the intravitreal administration of NMDA in murine models, observable signs of cell pyknosis emerge within just one hour. Subsequently, the associated Thy-1 mRNA levels in the retina commence a decline at the six-hour mark, culminating in the death of retinal ganglion cells approximately 24 hours post-injection.
- Optic Nerve Clamp Induced Optic Nerve Injury Models
Following the induction of anesthesia in the rat, the procedure progresses under a binocular surgical microscope: an incision is created at the lateral canthus. Subsequently, the Tenon's capsule is incised to expose the underlying structures. The lateral rectus muscle is then carefully isolated and transected. Employing blunt dissection techniques, the surgical field extends along the temporal scleral surface toward the optic nerve. A small vascular clamp is then strategically positioned on the optic nerve posterior to the globe for a specified period, thereby establishing a model of optic nerve crush injury in the rat.
- Hypertonic Saline Injection Models
Administering hypertonic saline into the episcleral veins induces sclerosis of the trabecular meshwork, thereby enhancing resistance to aqueous humor outflow and subsequently elevating intraocular pressure in experimental animal models. Utilizing a glass micropipette linked to a syringe, hypertonic saline is meticulously injected into the scleral vein of rats. Within a timeframe of 7 to 10 days post-injection, necrosis of the trabecular meshwork ensues, obstructing the aqueous humor's egress and resulting in heightened intraocular pressure. This elevation can be sustained for as long as 200 days.
- Spontaneous Glaucoma Mouse Models
The DBA/2J mouse model epitomizes the study of spontaneous glaucoma. In DBA/2J mice, apoptosis of retinal ganglion cells alongside optic nerve degeneration commences between 8 and 9 months of age. By the time these mice reach 18 months, over 90% of the optic nerve exhibits severe degeneration, with visual capabilities nearly entirely diminished. The apoptosis rate in retinal ganglion cells can exceed 90%, positioning DBA/2J mice as an exceptional experimental model for investigating glaucoma pathophysiology and potential therapeutic interventions.
- Anterior Chamber Injection Model
Injecting specific substances into the anterior chamber of experimental animals, such as sodium hyaluronate, methylcellulose, etc., increases the outflow resistance of aqueous humor or blocking the trabecular meshwork, thereby slowing or blocking the outflow of aqueous humor, resulting in increased intraocular pressure. A single injection of hyaluronic acid into the anterior chamber of rats for 5 days can form an acute high intraocular pressure model. If the injection is repeated once a week for 9 weeks, a chronic high intraocular pressure model can be formed.
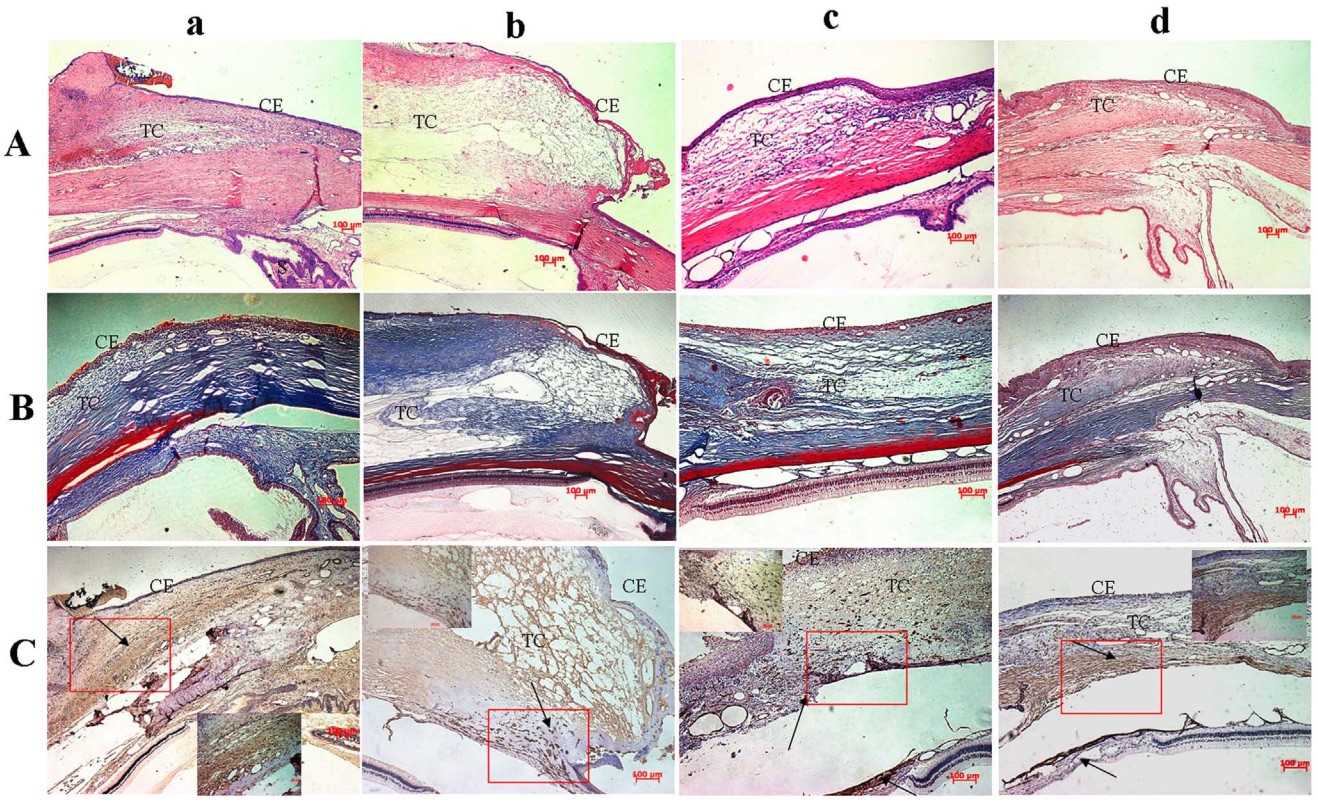 Fig 1. Histological images of rabbit glaucoma models.1
Fig 1. Histological images of rabbit glaucoma models.1
Measurements
Creative Biolabs' ophthalmology platform can provide a variety of testing services after drug administration in glaucoma models, such as:
- Lens opacity
- Intraocular pressure
- Optical coherence tomography
- Western blotting analysis (e.g. Tau, NOX1, NOX2, NOX4, NOXO1, p47PHOX)
- Histopathological observation (e.g., retina, optic nerve, cornea)
Related Ocular Disease Models
Furthermore, you may also be interested in other rodent ocular disease models, such as:
- Dry Eye Models
- Corneal Disease Models
- Cataract Models
- Dry Age-Related Macular Degeneration (AMD) Models
- Wet Age-Related Macular Degeneration (AMD) Models
- Fundus Disease Models
- Diabetic Retinopathy Models
- Retinal Fibrosis Models
- Retinal Vein Occlusion Models
- Ocular Inflammation Models
Creative Biolabs has established a comprehensive evaluation system for disease animal models. You can consult through the contact information on the company's home page.
Reference
- Xi, Lei, et al. "Evaluation of an injectable thermosensitive hydrogel as drug delivery implant for ocular glaucoma surgery." PLoS One 9.6 (2014): e100632. Distributed under Open Access license CC BY 4.0, without modification.
For Research Use Only.
