Salt induced Hypertentison Modeling & Pharmacodynamics Service in Dahl Salt-Sensitive Rat
At Creative Biolabs, we are dedicated to advancing the understanding and treatment of hypertension by providing a diverse array of meticulously validated preclinical models, enabling precise evaluation of novel compounds and therapeutic strategies.
Introduction
Hypertension, characterized by persistently elevated blood pressure, stands as a leading risk factor for severe cardiovascular events, including heart attack, stroke, and kidney failure. A significant subset of this condition, salt-sensitive hypertension, is directly influenced by dietary sodium intake, presenting unique challenges for therapeutic intervention.
Salt-Induced Hypertension Model in Dahl Salt-Sensitive Rats
The Dahl salt-sensitive (DSS) rat, a genetically predisposed model, reliably develops hypertension and significant end-organ damage (renal injury, cardiac hypertrophy, vascular remodeling) when exposed to a high-sodium diet. This model accurately mirrors human salt-sensitive hypertension, serving as an indispensable tool for deciphering mechanisms, validating therapeutic targets, and screening anti-hypertensive drugs. Its clear, quantifiable phenotype is ideal for robust preclinical investigations.
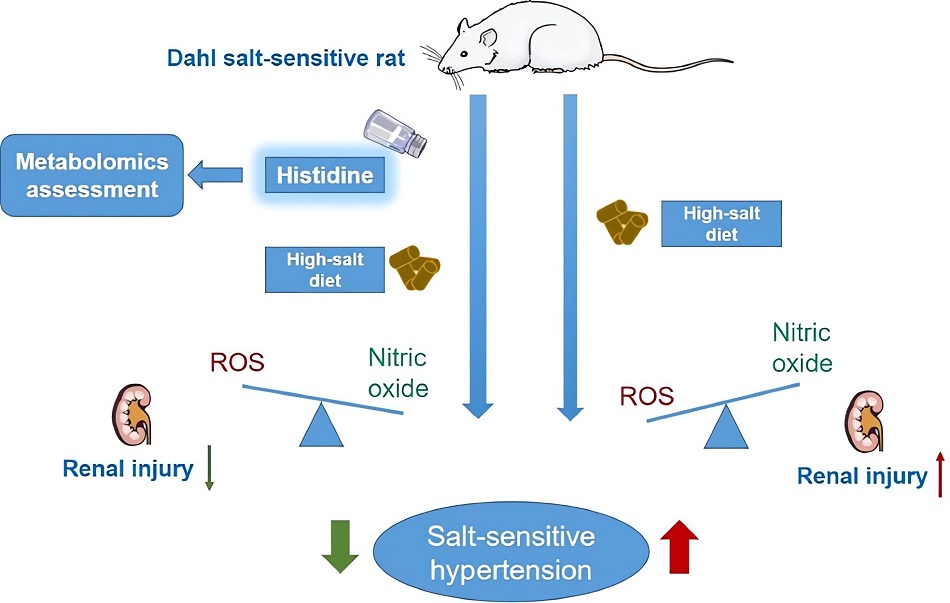 Fig.1 A research case of the DSS rat model.1,3
Fig.1 A research case of the DSS rat model.1,3
Model Construction Steps
The induction of salt-sensitive hypertension in Dahl rats involves a carefully controlled dietary regimen following their genetic predisposition. The model is established by providing DSS rats with a high-sodium diet over a defined period, leading to a reproducible and robust hypertensive phenotype.
01Animal Selection
Healthy DSS rats, typically weighing between 250-300g, are selected for the study.
02Dietary Intervention
Animals are transitioned to a high-salt diet (HSD), typically containing 2% to 4% NaCl, compared to a normal salt diet (0.3% to 0.5% NaCl) for control groups. This can be administered through specialized feed or by replacing drinking water with an 8% NaCl solution.
03Duration of Induction
The high-salt dietary intervention typically ranges from 2 to 8 weeks. Blood pressure elevation usually becomes evident within 1 to 4 weeks, often reaching systolic values between 160 and 180 mmHg.
04Monitoring
Blood pressure variations are regularly monitored using methods such as telemetry or tail-cuff measurements at predetermined intervals.
05Endpoint Assessment
At the study's conclusion, comprehensive assessments often include the removal and weighing of hearts to evaluate left and right ventricular hypertrophy, as well as total cardiac mass.
Strengths and Limitations
Strengths:
- Genetic Fidelity: Possesses an inherent genetic predisposition to salt-sensitive hypertension, closely resembling genetic components in human populations.
- Physiological Mimicry: Faithfully recapitulates the progressive nature of hypertension and associated end-organ damage, including renal injury and cardiac hypertrophy.
- Clear Phenotype: Exhibits a distinct and quantifiable blood pressure response to dietary sodium, facilitating robust therapeutic evaluations.
- Translational Relevance: Provides critical insights with high translational potential, informing clinical trials and drug development.
- Dietary Impact Nuance: Highly valuable for investigating the influence of various dietary compositions (beyond just salt concentration) on immune responses and disease progression.
Limitations:
- Multifactorial Complexity: While excellent for salt-sensitive hypertension, it may not encompass all the multifactorial etiologies of human essential hypertension.
- Irreversibility Challenges: Established hypertension and renal damage may not be fully reversible even after salt restriction, requiring specific strategies for evaluating late-stage interventions.
Evaluation Platform
Creative Biolabs provides a robust evaluation platform for the DSS rat model, ensuring precise and actionable data through integrated techniques.
Integrated Techniques: We combine biochemical, molecular, cellular, histopathological, behavioral, and advanced imaging methods.
Key Test Indicators:
- Physiological: Blood pressure (telemetry/tail-cuff), glomerular filtration rate (GFR), urine electrolyte excretion.
- Organ Function/Damage: Markers of kidney injury (e.g., proteinuria), cardiac hypertrophy and function (echocardiography, heart weight), vascular reactivity.
- Molecular/Cellular: Inflammatory markers, oxidative stress indicators, T-lymphocyte transcriptome profiling, and assessment of ENaC activity.
Applications
- Disease Simulation: Effectively simulates salt-sensitive hypertension, chronic hypertension with associated end-organ damage (renal failure, cardiac hypertrophy, vascular remodeling), and aspects of resistant hypertension.
- Drug Evaluation: Ideal for evaluating novel anti-hypertensive compounds, diuretics, agents targeting epithelial sodium channels (ENaC), anti-inflammatory drugs, and compounds influencing renal sodium handling or vascular function.
- Mechanism Elucidation: Crucial for unraveling the complex interplay of renal, sympathetic nervous system, inflammatory, and vascular mechanisms in hypertension.
- Therapeutic Strategy Development: Supports the development and validation of dietary interventions, pharmacological treatments, and combination therapies aimed at preventing or reversing salt-induced hypertension and its complications.
Related Hypertension Models
Our Advantages
- Extensive Expertise: Years leading preclinical hypertension research.
- Scientific Rigor: Our expert biologists and state-of-the-art facilities ensure unparalleled scientific precision.
- Customized Solutions: We design studies tailored to your exact objectives, from target validation to lead optimization.
- DSS Model Mastery: Deep understanding of the DSS model, including dietary impacts and disease irreversibility.
- Accelerated Discovery: Delivers highly relevant, translational data to expedite your drug development pipeline.
Work with Us
- Summarize the project requirements and fill in the information collection form.
- Sign a CDA from both parties to further communicate information, such as targets.
- Select an animal model, discuss experimental design, and determine assay parameters.
- Project costing and project schedule forecasting.
- We provide a detailed project plan, including the required sample quantities, methods, and protocols.
- Both parties confirm the project details and start the project.
- Confirm the timeline of the project.
- We provide periodic results and information on the animal's condition.
- We will work together to make project adjustments as necessary.
- We provide a comprehensive project report promptly.
- We arrange transportation for the produced samples.
- We provide a discussion of the project results and help to arrange the next steps.
- Data storage and archiving.
Contact Us
Creative Biolabs is committed to providing comprehensive, high-quality preclinical research services utilizing the DSS rat model. Our scientific expertise and advanced platforms are designed to guide your drug development journey. We invite you to contact us today to discuss how our tailored solutions can support your next breakthrough in hypertension research.
FAQs
-
Q1: Can the hypertension and renal damage in DSS rats be completely reversed by simply removing the high-salt diet once the condition is established?
A: Interestingly, studies indicate that established hypertension and associated renal damage, such as glomerular injury and proteinuria, in DSS rats may not be fully reversible even after the high-salt diet is withdrawn. This phenomenon, often referred to as a self-sustaining phase, highlights the model's utility in studying chronic and resistant forms of hypertension.
-
Q2: How do you ensure the reproducibility and consistency of results when conducting studies with dietary interventions in DSS rats?
A: Our approach involves rigorous control over all dietary parameters. We meticulously manage not only the precise sodium concentration (e.g., 2-4% NaCl for high-salt diets) but also the overall dietary composition, such as the distinction between purified and grain-fed diets. This comprehensive control is crucial because different dietary components can significantly influence immune responses and the progression of hypertension.
-
Q3: Is the DSS model more suitable for early-stage target validation or for evaluating late-stage drug efficacy in hypertension research?
A: The DSS model is versatile and suitable for both. Its well-defined genetic basis and clear hypertensive phenotype make it excellent for early-stage target validation. Furthermore, its capacity to develop chronic, self-sustaining hypertension and irreversible organ damage positions it as a robust model for evaluating the efficacy of compounds against established or resistant hypertension in later-stage drug development.
-
Q4: How does the DSS model contribute to understanding the multifactorial nature of human essential hypertension, given its focus on salt sensitivity?
A: While the DSS model primarily focuses on salt-induced hypertension, the pathological mechanisms it exhibits—including renal dysfunction, sympathetic nervous system activation, inflammation, and vascular remodeling—are broadly relevant to various forms of human hypertension. It provides a controlled environment to dissect the complex interplay of these factors, and can also be combined with other interventions to mimic additional comorbidities.
-
Q5: What are the key quantitative readouts and parameters that Creative Biolabs typically measures to assess drug efficacy in studies involving DSS rats?
A: Our efficacy assessments rely on a comprehensive set of quantitative readouts. These include continuous blood pressure monitoring, measurements of proteinuria, evaluation of cardiac and renal hypertrophy, assessment of glomerular filtration rate, analysis of urine electrolyte excretion, quantification of inflammatory and oxidative stress biomarkers, and functional characterization of vascular responses.
-
Q6: What is the primary translational relevance of findings from the DSS rat model to human hypertension and therapeutic development?
A: The DSS model offers direct translational relevance to human salt-sensitive hypertension, a significant clinical challenge. Insights gained from this model contribute to understanding the progression of chronic and resistant hypertension, identifying persistent pathological mechanisms (such as ENaC hyperactivity), and validating novel therapeutic targets that can lead to more effective treatments for patients.
Published Data
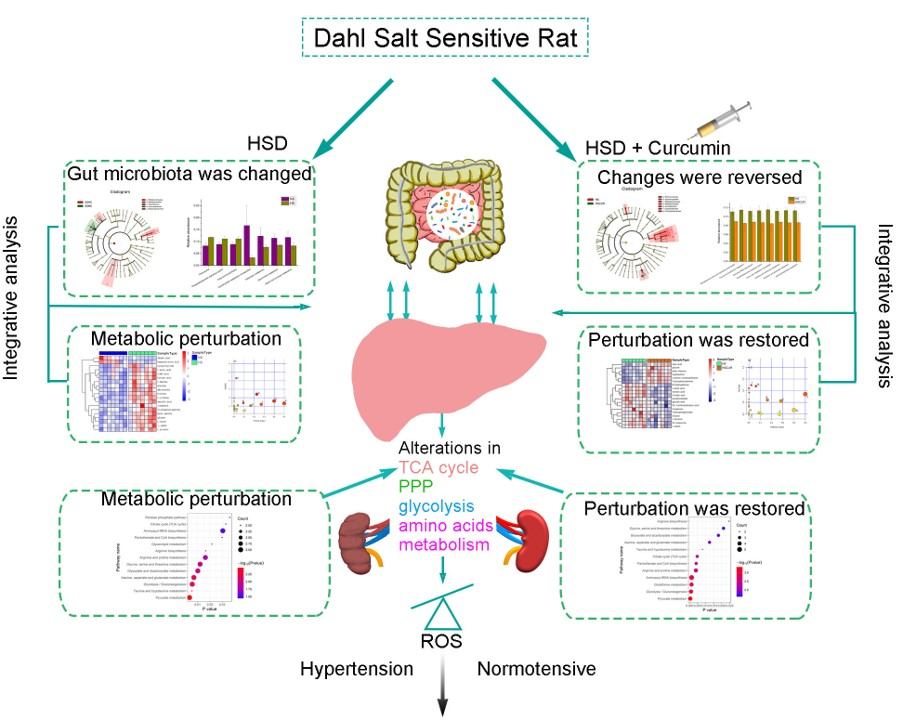 Fig.2 Pathogenesis of salt-sensitive hypertension in DSS rats.2,3
Fig.2 Pathogenesis of salt-sensitive hypertension in DSS rats.2,3
A compelling study utilized integrated multi-omics analysis to investigate the pathogenesis of salt-sensitive hypertension in DSS rats. The research demonstrated that a high-salt diet induced significant metabolic dysfunction, particularly impacting amino acid metabolism pathways related to glycolysis. Furthermore, the study identified alterations in the gut microbiota and hepatic metabolism as key extra-renal mechanisms contributing to the disease. This work highlights the complex interplay of the gut-liver axis and metabolic reprogramming in salt-induced hypertension, suggesting novel therapeutic avenues beyond traditional targets.
References
- Bhat, Mehvish, et al. "A current review on animal models of anti-hypertensive drugs screening." Health Sciences Review 6 (2023). https://doi.org/10.1016/j.hsr.2023.100078.
- Ou-Yang, Ya-Nan et al. "Revealing the Pathogenesis of Salt-Sensitive Hypertension in Dahl Salt-Sensitive Rats through Integrated Multi-Omics Analysis." Metabolites vol. 12,11 1076. 7 Nov. 2022. https://doi.org/10.3390/metabo12111076
- Distributed under Open Access license CC BY 4.0, without modification.
For Research Use Only.
