Contrast Agent induced Acute Kidney Injury Modeling & Pharmacodynamics Service
Creative Biolabs offers a reliable contrast agent-induced acute kidney injury model to assess renal injury and evaluate therapeutic interventions efficiently, offering accurate results for drug discovery and preclinical research.
Introduction
Acute Kidney Injury (AKI) refers to a sudden and rapid decline in kidney function, leading to the accumulation of waste products, fluid retention, and electrolyte imbalances. AKI can result from various factors, including ischemia, toxins, infections, and drug-induced damage, with contrast-induced nephropathy (CIN) being one of the leading causes in hospitalized patients. The clinical manifestation of AKI includes a rise in serum creatinine, reduced urine output, and disturbances in fluid balance, which can lead to severe complications such as multi-organ failure and even death if not properly managed. AKI is often reversible with early detection and intervention, but it can progress to chronic kidney disease (CKD) if not treated appropriately. In clinical settings, patients undergoing imaging procedures involving contrast agents are particularly at risk of developing contrast-induced AKI, which further emphasizes the importance of early diagnosis and therapeutic strategies. Given the complexity and varied etiology of AKI, animal models are essential for investigating the pathophysiological mechanisms and developing effective treatment strategies.
Contrast Agent-Induced Acute Kidney Injury Model
The contrast agent-induced acute kidney injury model is established by administering high doses of contrast agents, such as iodinated contrast, to rodents. This method mimics the renal toxicity seen in patients undergoing imaging procedures. The model allows researchers to evaluate the onset of renal injury, the role of oxidative stress, and the effect of pharmacological interventions. The primary advantage of this model lies in its ability to reproduce the clinical manifestations of contrast-induced nephropathy, including elevated serum creatinine and histological damage to the renal tubules. However, one limitation is that the model might not fully replicate the long-term effects seen in humans with chronic kidney disease.
- Simulates: This model simulates contrast agent-induced nephropathy, a form of acute kidney injury, providing a valuable tool for understanding the underlying mechanisms and the early stages of renal dysfunction caused by contrast media.
- Evaluates Drugs: This model is highly effective for evaluating drugs aimed at protecting against contrast-induced kidney injury, such as antioxidants, vasodilators, and renoprotective agents. It also allows for testing the efficacy of therapies that may help reverse the damage caused by contrast agents.
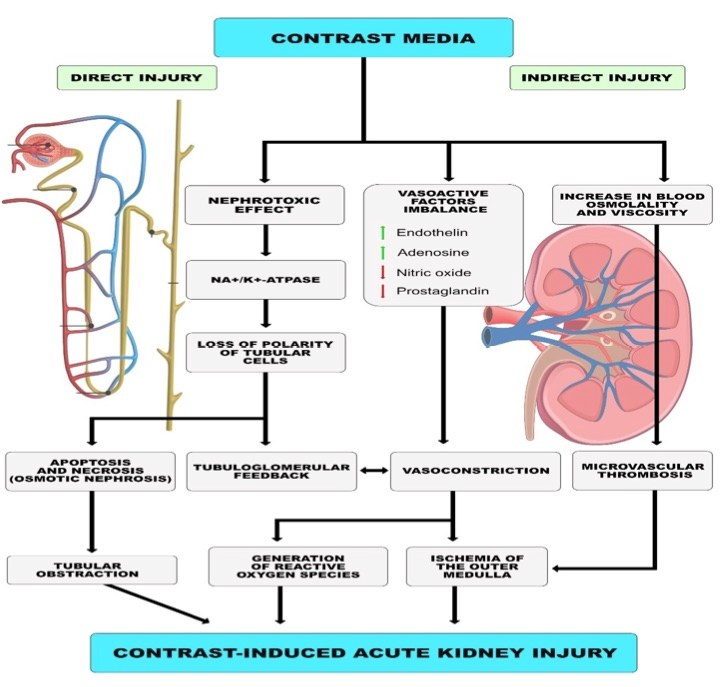 Fig. 1 Proposed mechanism of contrast-induced acute kidney injury.1,3
Fig. 1 Proposed mechanism of contrast-induced acute kidney injury.1,3
Evaluation Platform
- Animals: Mouse, Rat, Hamster, Rabbit, Cat, Dog, NHPs.
-
Measurements
We offer a wide range of measurements for evaluating drug efficacy in this model, utilizing cutting-edge technologies such as:- General observations: Body weight, mortality rate, and changes in renal function, including serum creatinine and blood urea nitrogen (BUN) levels.
- Histopathological analysis: Hematoxylin and eosin (H&E) staining to observe renal tubule damage, interstitial fibrosis, and glomerular abnormalities.
- Biomarker profiling (e.g., ELISA): Levels of kidney injury markers such as KIM-1, NGAL, and Cystatin C.
- Cytokine profiling: Expression of pro-inflammatory cytokines (e.g., TNF-α, IL-1β) and markers of oxidative stress.
- Gene/protein expression profiling: Quantitative PCR and Western blot analysis to measure renal injury-related genes and proteins.
In addition to these standard assays, we can tailor experimental designs to focus on specific mechanisms or pathways relevant to your research.
Related Services
In addition to the contrast agent-induced model, we offer a variety of other methods for inducing acute kidney injury, such as those using cisplatin, glycerol, and ischemia-reperfusion injury. Each method is suited for different research objectives, providing a comprehensive range of options for AKI studies.
- Gentamicin-Induced Acute Renal Failure Model
- Cisplatin-Induced Acute Renal Injury Model
- Glycerol-Induced Acute Renal Failure Model
- Folic Acid-Induced Acute Kidney Injury Model
- Lipopolysaccharide (LPS)-Induced Acute Kidney Injury Model
- Cecal Ligation and Puncture (CLP)-Induced Acute Kidney Injury Model
Our advantages
- Tailored research support: Our scientific team works closely with clients to design customized experiments, ensuring the best approach for your research goals.
- State-of-the-art facilities: We use advanced technologies for biomarker analysis, histology, and gene/protein expression studies.
- Reproducible results: Our models provide highly reproducible data, enabling reliable evaluation of drug efficacy and mechanism of action.
- Diverse model options: We offer various AKI models, allowing researchers to select the one most suited to their specific needs.
- Expert consultation: Our team is available to assist in experimental design, troubleshooting, and data interpretation throughout the study process.
Work with Us
- Summarize the project requirements and fill in the information collection form.
- Sign a CDA from both parties to further communicate information, such as targets.
- Select an animal model, discuss experimental design, and determine assay parameters.
- Project costing and project schedule forecasting.
- We provide a detailed project plan, including the required sample quantities, methods, and protocols.
- Both parties confirm the project details and start the project.
- Confirm the timeline of the project.
- We provide periodic results and information on the animal's condition.
- We will work together to make project adjustments as necessary.
- We provide a comprehensive project report promptly.
- We arrange transportation for the produced samples.
- We provide a discussion of the project results and help to arrange the next steps.
- Data storage and archiving.
FAQs
-
1. What is the duration of the study for the contrast agent-induced AKI model?
Studies typically last 7 to 14 days, depending on the severity of kidney injury and the therapeutic interventions being tested.
-
2. What types of contrast agents are used in this model?
We use iodinated contrast agents, commonly used in clinical imaging, to induce kidney injury.
-
3. Can this model be used to test both preventative and therapeutic treatments?
Yes, it is suitable for evaluating both prophylactic treatments to prevent kidney injury and therapeutic agents aimed at reversing renal damage.
-
4. Are there any limitations to this model?
While it replicates the early stages of contrast-induced nephropathy, it may not fully recapitulate the long-term progression seen in patients with chronic kidney disease.
Published Data
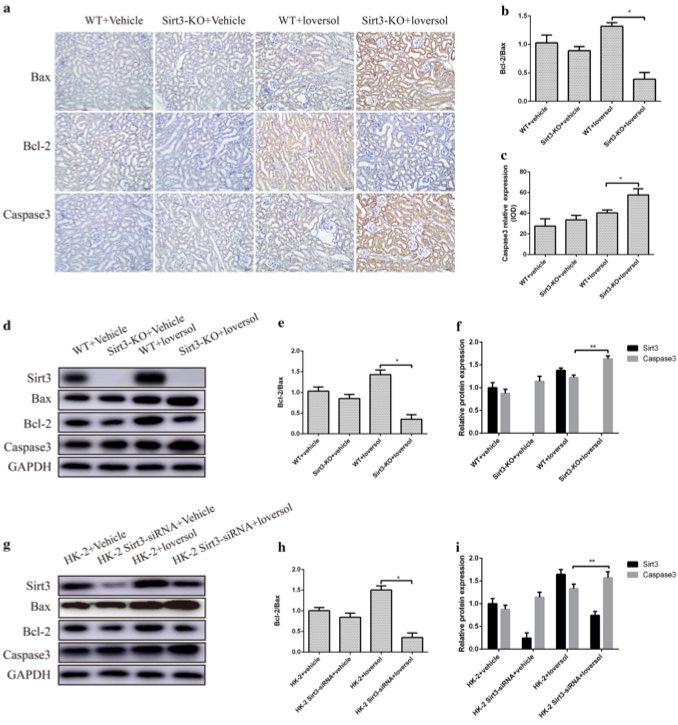 Fig. 2 Sirt3 deficiency increased apoptosis in contrast-induced acute kidney injury.2,3
Fig. 2 Sirt3 deficiency increased apoptosis in contrast-induced acute kidney injury.2,3
Sirt3 was found to have a protective effect against apoptosis in the contrast-induced acute kidney injury (CIAKI) model. Apoptosis in the kidney is associated with the severity of acute kidney injury (AKI). To explore the role of Sirt3 in CIAKI, the expression of apoptotic and antiapoptotic proteins was evaluated. Immunohistochemical analysis of Bax, Bcl-2, and Caspase-3 expression in kidney tissues revealed that Caspase-3 expression was significantly elevated in Sirt3 knockout (Sirt3-KO) mice following Ioversol treatment, with statistically significant differences compared to wild-type (WT) mice. Moreover, Sirt3 deficiency resulted in a significant reduction in the Bcl-2/Bax ratio in Ioversol-treated mice (Fig. 2a–c). Western blot analysis corroborated these findings (Fig. 2d–f). In addition, similar results were observed in HK-2 cells (Fig. 2g–i). These findings collectively demonstrate that Sirt3 deficiency exacerbates apoptosis in the kidneys of the CIAKI model.
References
- Maksimczuk, Joanna et al. "What Promotes Acute Kidney Injury in Patients with Myocardial Infarction and Multivessel Coronary Artery Disease-Contrast Media, Hydration Status or Something Else?" Nutrients vol. 15,1 21. 21 Dec. 2022. https://doi.org/10.3390/nu15010021
- Zhang, Qinghai et al. "Sirtuin 3 deficiency aggravates contrast-induced acute kidney injury." Journal of translational medicine vol. 16,1 313. 16 Nov. 2018. https://doi.org/10.1186/s12967-018-1690-5
- Distributed under Open Access license CC BY 4.0, without modification.
For Research Use Only.
